Suicide Protection
Suicide is a serious public health problem that can have lasting harmful effects on individuals, families, and communities. While its causes are complex and determined by multiple factors, the goal of suicide prevention is simple: Reduce factors that increase risk (i.e. risk factors) and increase factors that promote resilience (i.e. protective factors). Ideally, prevention addresses all levels of influence: individual, relationship, community, and societal. Effective prevention strategies are needed to promote awareness of suicide and encourage a commitment to social change.
Suicide, like all human behavior, results from a confluence of different and sometimes conflicting purposes. So many are hurting for one reason or another. Social media is very popular but seems to help embolden more and more, to take their own life.
The one question everyone has asked without exception, that they ache to have answered more than any other, is simply, why?
Why did their friend, child, parent, spouse, or sibling take their own life? Even when a note explaining the reasons is found, lingering questions usually remain: yes, they felt enough despair to want to die, but why did they feel that? A person’s suicide often takes the people it leaves behind by surprise (only accentuating survivor’s guilt for failing to see it coming).
In general, people try to kill themselves for six reasons:
Suicide, like all human behavior, results from a confluence of different and sometimes conflicting purposes. So many are hurting for one reason or another. Social media is very popular but seems to help embolden more and more, to take their own life.
The one question everyone has asked without exception, that they ache to have answered more than any other, is simply, why?
Why did their friend, child, parent, spouse, or sibling take their own life? Even when a note explaining the reasons is found, lingering questions usually remain: yes, they felt enough despair to want to die, but why did they feel that? A person’s suicide often takes the people it leaves behind by surprise (only accentuating survivor’s guilt for failing to see it coming).
In general, people try to kill themselves for six reasons:
Definitions: Self-directed Violence
- Suicide
Death caused by self-directed injurious behavior with an intent to die as a result of the behavior. - Suicide attempt
A non-fatal, self-directed, potentially injurious behavior with an intent to die as a result of the behavior; might not result in injury. - Suicidal ideation
Thinking about, considering, or planning suicide.
Suicide: Risk and Protective Factors
On This Page
Risk Factors for Suicide
A combination of individual, relationship, community, and societal factors contribute to the risk of suicide. Risk factors are those characteristics associated with suicide—they might not be direct causes.
Know the Risk Factors
Risk factors are characteristics that make it more likely that someone will consider, attempt, or die by suicide. They can't cause or predict a suicide attempt, but they're important to be aware of.
•Mental disorders, particularly mood disorders, schizophrenia, anxiety disorders, and certain personality disorders
•Alcohol and other substance use disorders
•Hopelessness
•Impulsive and/or aggressive tendencies
•History of trauma or abuse
•Major physical illnesses
•Previous suicide attempt(s)
•Family history of suicide
Family history of child maltreatment
•Job or financial loss
•Loss of relationship(s)
Impulsive or aggressive tendencies
•Easy access to lethal means
•Local clusters of suicide
•Lack of social support and sense of isolation
•Unwillingness to seek help because of the stigma attached to mental health and substance abuse disorders or to suicidal thoughts
•Lack of healthcare, especially mental health and substance abuse treatment
•Cultural and religious beliefs, such as the belief that suicide is a noble resolution of a personal dilemma
•Exposure to others who have died by suicide (in real life or via the media and Internet)
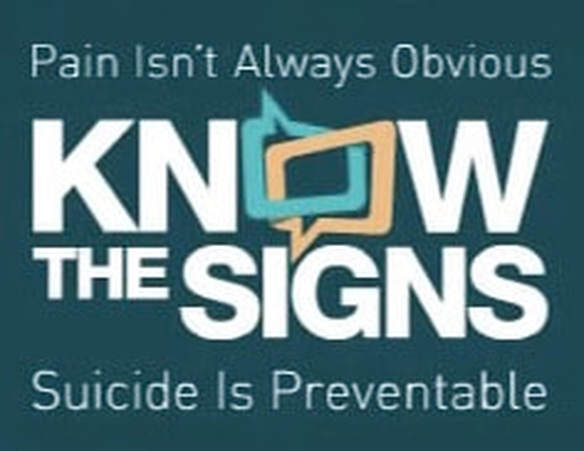
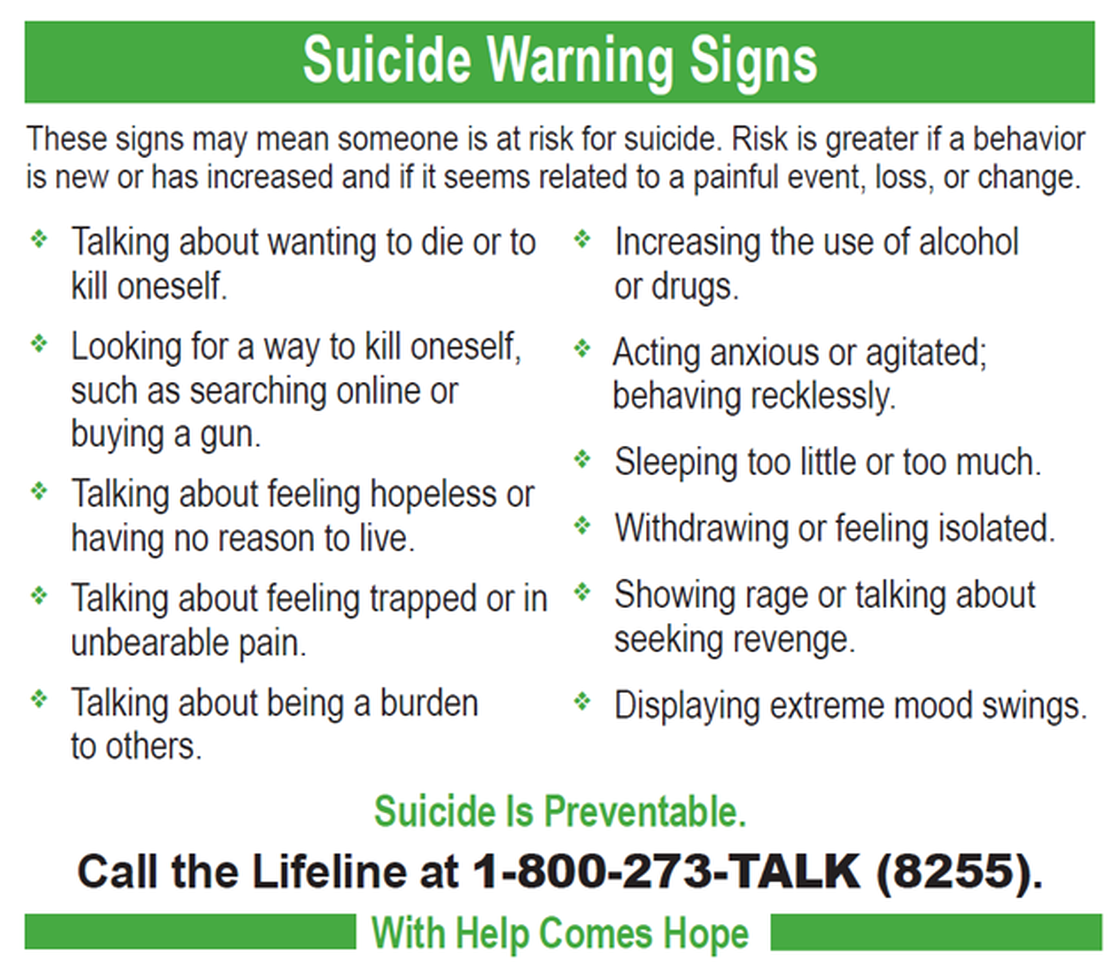
Know the Warning Signs
Some warning signs may help you determine if a loved one is at risk for suicide, especially if the behavior is new, has increased, or seems related to a painful event, loss, or change. If you or someone you know exhibits any of these, seek help by calling the Lifeline.
•Talking about wanting to die or to kill themselves
•Looking for a way to kill themselves, like searching online or buying a gun
•Talking about feeling hopeless or having no reason to live
•Talking about feeling trapped or in unbearable pain
•Talking about being a burden to others
•Increasing the use of alcohol or drugs
•Acting anxious or agitated; behaving recklessly
•Sleeping too little or too much
•Withdrawing or isolating themselves
•Showing rage or talking about seeking revenge
•Extreme mood swings
Protective Factors for Suicide
Protective factors buffer individuals from suicidal thoughts and behavior. To date, protective factors have not been studied as extensively or rigorously as risk factors. Identifying and understanding protective factors are, however, equally as important as researching risk factors.
Protective Factors
On This Page
Risk Factors for Suicide
A combination of individual, relationship, community, and societal factors contribute to the risk of suicide. Risk factors are those characteristics associated with suicide—they might not be direct causes.
Know the Risk Factors
Risk factors are characteristics that make it more likely that someone will consider, attempt, or die by suicide. They can't cause or predict a suicide attempt, but they're important to be aware of.
•Mental disorders, particularly mood disorders, schizophrenia, anxiety disorders, and certain personality disorders
•Alcohol and other substance use disorders
•Hopelessness
•Impulsive and/or aggressive tendencies
•History of trauma or abuse
•Major physical illnesses
•Previous suicide attempt(s)
•Family history of suicide
Family history of child maltreatment
•Job or financial loss
•Loss of relationship(s)
Impulsive or aggressive tendencies
•Easy access to lethal means
•Local clusters of suicide
•Lack of social support and sense of isolation
•Unwillingness to seek help because of the stigma attached to mental health and substance abuse disorders or to suicidal thoughts
•Lack of healthcare, especially mental health and substance abuse treatment
•Cultural and religious beliefs, such as the belief that suicide is a noble resolution of a personal dilemma
•Exposure to others who have died by suicide (in real life or via the media and Internet)
Know the Warning Signs
Some warning signs may help you determine if a loved one is at risk for suicide, especially if the behavior is new, has increased, or seems related to a painful event, loss, or change. If you or someone you know exhibits any of these, seek help by calling the Lifeline.
•Talking about wanting to die or to kill themselves
•Looking for a way to kill themselves, like searching online or buying a gun
•Talking about feeling hopeless or having no reason to live
•Talking about feeling trapped or in unbearable pain
•Talking about being a burden to others
•Increasing the use of alcohol or drugs
•Acting anxious or agitated; behaving recklessly
•Sleeping too little or too much
•Withdrawing or isolating themselves
•Showing rage or talking about seeking revenge
•Extreme mood swings
Protective Factors for Suicide
Protective factors buffer individuals from suicidal thoughts and behavior. To date, protective factors have not been studied as extensively or rigorously as risk factors. Identifying and understanding protective factors are, however, equally as important as researching risk factors.
Protective Factors
- Effective clinical care for mental, physical, and substance abuse disorders
- Easy access to a variety of clinical interventions and support for help seeking
- Family and community support (connectedness)
- Support from ongoing medical and mental health care relationships
- Skills in problem solving, conflict resolution, and nonviolent ways of handling disputes
- Cultural and religious beliefs that discourage suicide and support instincts for self-preservation
1. They’re depressed.
This is without question the most common reason people commit suicide. Severe depression is always accompanied by a pervasive sense of suffering as well as the belief that escape from it is hopeless. The pain of existence often becomes too much for severely depressed people to bear. The state of depression warps their thinking, allowing ideas like “Everyone would all be better off without me” to make rational sense. They shouldn’t be blamed for falling prey to such distorted thoughts any more than a heart patient should be blamed for experiencing chest pain: it’s simply the nature of their disease.
Because depression, as we all know, is almost always treatable, we should all seek to recognize its presence in our close friends and loved ones. Often people suffer with it silently, planning suicide without anyone ever knowing. Despite making both parties uncomfortable, inquiring directly about suicidal thoughts in my experience almost always yields a honest response. If you suspect someone might be depressed, don’t allow your tendency to deny the possibility of suicidal ideation prevent you from asking about it.
This is without question the most common reason people commit suicide. Severe depression is always accompanied by a pervasive sense of suffering as well as the belief that escape from it is hopeless. The pain of existence often becomes too much for severely depressed people to bear. The state of depression warps their thinking, allowing ideas like “Everyone would all be better off without me” to make rational sense. They shouldn’t be blamed for falling prey to such distorted thoughts any more than a heart patient should be blamed for experiencing chest pain: it’s simply the nature of their disease.
Because depression, as we all know, is almost always treatable, we should all seek to recognize its presence in our close friends and loved ones. Often people suffer with it silently, planning suicide without anyone ever knowing. Despite making both parties uncomfortable, inquiring directly about suicidal thoughts in my experience almost always yields a honest response. If you suspect someone might be depressed, don’t allow your tendency to deny the possibility of suicidal ideation prevent you from asking about it.
2. They’re psychotic.
Malevolent inner voices often command self-destruction for unintelligible reasons. Psychosis is much harder to mask than depression — and arguably even more tragic. The worldwide incidence of schizophrenia is 1% and often strikes otherwise healthy, high-performing individuals, whose lives, though manageable with medication, never fulfill their original promise.
Schizophrenics are just as likely to talk freely about the voices commanding them to kill themselves as not, and also, in my experience, give honest answers about thoughts of suicide when asked directly. Psychosis, too, is treatable and usually must be for a schizophrenic to be able to function at all. Untreated or poorly treated psychosis almost always requires hospital admission to a locked ward until the voices lose their commanding power.
3. They’re impulsive.
Often related to drugs and alcohol, some people become maudlin and impulsively attempt to end their own lives. Once sobered and calmed, these people usually feel emphatically ashamed. The remorse is usually genuine, and whether or not they’ll ever attempt suicide again is unpredictable. They may try it again the very next time they become drunk or high, or never again in their lifetime. Hospital admission is, therefore, not usually indicated. Substance abuse and the underlying reasons for it are generally a greater concern in these people and should be addressed as aggressively as possible.
Malevolent inner voices often command self-destruction for unintelligible reasons. Psychosis is much harder to mask than depression — and arguably even more tragic. The worldwide incidence of schizophrenia is 1% and often strikes otherwise healthy, high-performing individuals, whose lives, though manageable with medication, never fulfill their original promise.
Schizophrenics are just as likely to talk freely about the voices commanding them to kill themselves as not, and also, in my experience, give honest answers about thoughts of suicide when asked directly. Psychosis, too, is treatable and usually must be for a schizophrenic to be able to function at all. Untreated or poorly treated psychosis almost always requires hospital admission to a locked ward until the voices lose their commanding power.
3. They’re impulsive.
Often related to drugs and alcohol, some people become maudlin and impulsively attempt to end their own lives. Once sobered and calmed, these people usually feel emphatically ashamed. The remorse is usually genuine, and whether or not they’ll ever attempt suicide again is unpredictable. They may try it again the very next time they become drunk or high, or never again in their lifetime. Hospital admission is, therefore, not usually indicated. Substance abuse and the underlying reasons for it are generally a greater concern in these people and should be addressed as aggressively as possible.
4. They’re crying out for help and don’t know how else to get it.
These people don’t usually want to die but do want to alert those around them that something is seriously wrong. They often don’t believe they will die, frequently choosing methods they don’t think can kill them in order to strike out at someone who’s hurt them—but are sometimes tragically misinformed. The prototypical example of this is a young teenage girl suffering genuine angst because of a relationship, either with a friend, boyfriend, or parent who swallows a bottle of Tylenol—not realizing that in high enough doses Tylenol causes irreversible liver damage.
I’ve watched more than one teenager die a horrible death in an ICU days after such an ingestion when remorse has already cured them of their desire to die and their true goal of alerting those close to them of their distress has been achieved.
5. They have a philosophical desire to die.
The decision to commit suicide for some is based on a reasoned decision often motivated by the presence of a painful terminal illness from which little to no hope of reprieve exists. These people aren’t depressed, psychotic, maudlin, or crying out for help. They’re trying to take control of their destiny and alleviate their own suffering, which usually can only be done in death. They often look at their choice to commit suicide as a way to shorten a dying that will happen regardless. In my personal view, if such people are evaluated by a qualified professional who can reliably exclude the other possibilities for why suicide is desired, these people should be allowed to die at their own hands.
These people don’t usually want to die but do want to alert those around them that something is seriously wrong. They often don’t believe they will die, frequently choosing methods they don’t think can kill them in order to strike out at someone who’s hurt them—but are sometimes tragically misinformed. The prototypical example of this is a young teenage girl suffering genuine angst because of a relationship, either with a friend, boyfriend, or parent who swallows a bottle of Tylenol—not realizing that in high enough doses Tylenol causes irreversible liver damage.
I’ve watched more than one teenager die a horrible death in an ICU days after such an ingestion when remorse has already cured them of their desire to die and their true goal of alerting those close to them of their distress has been achieved.
5. They have a philosophical desire to die.
The decision to commit suicide for some is based on a reasoned decision often motivated by the presence of a painful terminal illness from which little to no hope of reprieve exists. These people aren’t depressed, psychotic, maudlin, or crying out for help. They’re trying to take control of their destiny and alleviate their own suffering, which usually can only be done in death. They often look at their choice to commit suicide as a way to shorten a dying that will happen regardless. In my personal view, if such people are evaluated by a qualified professional who can reliably exclude the other possibilities for why suicide is desired, these people should be allowed to die at their own hands.
6. They’ve made a mistake.
This is a recent, tragic phenomenon in which typically young people flirt with oxygen deprivation for the high it brings and simply go too far. Or a grown man shoots himself while trying to clean a gun. The only defense against this, it seems to me, is education.
The wounds suicide leaves in the lives of those left behind by it are often deep and long lasting. The apparent senselessness of suicide often fuels the most significant pain survivors feel. Thinking we all deal better with tragedy when we understand its underpinnings, I’ve offered the preceding paragraphs in hopes that anyone reading this who’s been left behind by a suicide might be able to more easily find a way to move on, to relinquish their guilt and anger, and find closure. Despite the abrupt way you may have been left, those don’t have to be the only two emotions you’re doomed to feel about the one who left you.
Excerpted from: http://www.kevinmd.com/blog/2010/06/6-reasons-people-commit-suicide.html
This is a recent, tragic phenomenon in which typically young people flirt with oxygen deprivation for the high it brings and simply go too far. Or a grown man shoots himself while trying to clean a gun. The only defense against this, it seems to me, is education.
The wounds suicide leaves in the lives of those left behind by it are often deep and long lasting. The apparent senselessness of suicide often fuels the most significant pain survivors feel. Thinking we all deal better with tragedy when we understand its underpinnings, I’ve offered the preceding paragraphs in hopes that anyone reading this who’s been left behind by a suicide might be able to more easily find a way to move on, to relinquish their guilt and anger, and find closure. Despite the abrupt way you may have been left, those don’t have to be the only two emotions you’re doomed to feel about the one who left you.
Excerpted from: http://www.kevinmd.com/blog/2010/06/6-reasons-people-commit-suicide.html
Have the Conversation
Be the one to save a life. Use the #BeThe1To 5 action steps to help someone in your life that might be in crisis, or share the steps with others. These steps have been proven to help others find hope and support.
1. Ask
Research shows people who are having thoughts of suicide feel relief when someone asks after them in a caring way. Findings suggest acknowledging and talking about suicide may reduce suicidal ideation.
Be the one to save a life. Use the #BeThe1To 5 action steps to help someone in your life that might be in crisis, or share the steps with others. These steps have been proven to help others find hope and support.
1. Ask
Research shows people who are having thoughts of suicide feel relief when someone asks after them in a caring way. Findings suggest acknowledging and talking about suicide may reduce suicidal ideation.
2. Keep Them Safe
A number of studies have indicated that when lethal means are made less available or less deadly, suicide rates by that method decline, and frequently suicide rates overall decline.
A number of studies have indicated that when lethal means are made less available or less deadly, suicide rates by that method decline, and frequently suicide rates overall decline.
3. Be There
Individuals are more likely to feel less depressed, less suicidal, less overwhelmed, and more hopeful by after speaking to someone who listens without judgment.
Individuals are more likely to feel less depressed, less suicidal, less overwhelmed, and more hopeful by after speaking to someone who listens without judgment.
4. Help Them Connect
Studies indicate that helping someone at risk create a network of resources and individuals for support and safety can help them take positive action and reduce feelings of hopelessness.
Studies indicate that helping someone at risk create a network of resources and individuals for support and safety can help them take positive action and reduce feelings of hopelessness.
5. Follow Up
Studies have also shown that brief, low cost intervention and supportive, ongoing contact may be an important part of suicide prevention, especially for individuals after they have been discharged from hospitals or care services.
Studies have also shown that brief, low cost intervention and supportive, ongoing contact may be an important part of suicide prevention, especially for individuals after they have been discharged from hospitals or care services.
6. We Can All Prevent Suicide
Understanding the issues concerning suicide and mental health is an important way to take part in suicide prevention, help others in crisis, and change the conversation around suicide.
We Believe. Hope Can Happen.
Suicide is not inevitable for anyone. By starting the conversation, providing support, and directing help to those who need it, we can prevent suicides and save lives.
We Can All Take Action.
Evidence shows that providing support services, talking about suicide, reducing access to means of self-harm, and following up with loved ones are just some of the actions we can all take to help others.
By offering immediate counseling to everyone that may need it, local crisis centers provide invaluable support at critical times and connect individuals to local services.
Know the Risk Factors
Get in touch.
Call the Lifeline.
Call the Lifeline Anytime, 24/7
1-800-273-8255
Talk To Someone Now
Share.
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support,
the Lifeline network is available 24/7 across the United States.
The Lifeline is available for everyone, is free, and confidential.
National Suicide Prevention Lifeline
1-800-273-8255
Chat with Lifeline
Should I Call The Lifeline?
No matter what problems you’re dealing with, whether or not you’re thinking about suicide, if you need someone to lean on for emotional support, call the Lifeline.
People call to talk about lots of things: substance abuse, economic worries, relationships, sexual identity, getting over abuse, depression, mental and physical illness, and loneliness, to name a few.
Talking with someone about your thoughts and feelings can save your life.
Get in touch
Call the Lifeline
Call the Lifeline Anytime, 24/7
1-800-273-8255
Just Breathe
Understanding the issues concerning suicide and mental health is an important way to take part in suicide prevention, help others in crisis, and change the conversation around suicide.
We Believe. Hope Can Happen.
Suicide is not inevitable for anyone. By starting the conversation, providing support, and directing help to those who need it, we can prevent suicides and save lives.
We Can All Take Action.
Evidence shows that providing support services, talking about suicide, reducing access to means of self-harm, and following up with loved ones are just some of the actions we can all take to help others.
By offering immediate counseling to everyone that may need it, local crisis centers provide invaluable support at critical times and connect individuals to local services.
Know the Risk Factors
Get in touch.
Call the Lifeline.
Call the Lifeline Anytime, 24/7
1-800-273-8255
Talk To Someone Now
Share.
If you’re thinking about suicide, are worried about a friend or loved one, or would like emotional support,
the Lifeline network is available 24/7 across the United States.
The Lifeline is available for everyone, is free, and confidential.
National Suicide Prevention Lifeline
1-800-273-8255
Chat with Lifeline
Should I Call The Lifeline?
No matter what problems you’re dealing with, whether or not you’re thinking about suicide, if you need someone to lean on for emotional support, call the Lifeline.
People call to talk about lots of things: substance abuse, economic worries, relationships, sexual identity, getting over abuse, depression, mental and physical illness, and loneliness, to name a few.
Talking with someone about your thoughts and feelings can save your life.
Get in touch
Call the Lifeline
Call the Lifeline Anytime, 24/7
1-800-273-8255
Just Breathe
A wise professor once said to his class regarding suicide: There is never a wrong time, or a wrong way, to talk to someone about whether they’re thinking of killing themselves. If you suspect it, address it.
The Anxiety, Depression & Sleep Connection
It is important to remember that anxiety, depression and sleep disorders are all inter-connected. They are all causes and effects of each other, which can put someone into a downward spiral fast. Sadly, once the cycle starts, it can be challenging to stop. (13)
This is why you might want to consider using some of the essential oils that are traditionally used for insomnia and sleep disturbances in your anti-anxiety protocols. You’ll notice that several of the below oils are repeated from the list above, which suggests that these oils are particularly helpful: (10)
How to Use Essential Oils for Anxiety
There are several natural therapies that can help quiet your mind and calm your anti-anxiety. Let's discuss some useful applications and essential oil combinations.
Diffusion – the easiest and arguably the most effective approach to use essential oils for anxiety is to put a few drops of any of these oils above (or a homemade blend) in your diffuser before you go to bed. Some nice diffuser blends you might want to try are:
Topical – another effective strategy is to simply apply these key oils over certain parts of the body – particularly the trigger points – like the bottoms of the feet, on the wrists, behind the knees, behind the ears on the mastoid bone or on the back of the neck.
Be sure to use with a good carrier oil, and creating a 2-3% dilution is considered safe by most experts. For example,
If working with tablespoons is more comfortable for you, 1 oz. = 2 tablespoons. So, there are 300 drops of EO in a tablespoon.
Misting Spray – another great trick is to make a DIY Anxiety Spray. Using some of the same oils above:
Mist into the air and take in a deep breath during panic attacks, stressful moments or when anxiety settles in.
Other DIY Hacks – try making your favorite DIY recipes with these calming essential oils. It's a great way to calm the body and the mind. Here are some recipes for you – remember, just use the oils and blends above to give you the desired result:
Safety & Contraindications
Are you sure you're using essential oils safely and effectively? Are you confused by dilutions and conversions?
Take out the guesswork and download FREE roller bottle guide HERE.
This is why you might want to consider using some of the essential oils that are traditionally used for insomnia and sleep disturbances in your anti-anxiety protocols. You’ll notice that several of the below oils are repeated from the list above, which suggests that these oils are particularly helpful: (10)
- Angelica archangelica rad. (angelica)
- Cananga odorata (ylang ylang)
- Chamaemelum nobile (Roman chamomile)
- Citrus aurantium var. amara (neroli bigarade)
- Cistus ladaniferus (labdanum)
- Citrus bergamia (bergamot)
- limon (lemon)
- Citrus reticulata (mandarin)
- Citrus sinensis (sweet orange)
- Cuminum cyminum (cumin)
- Juniperus communis fruct. (juniper berry)
- Lavandula angustifolia (lavender)
- Litsea cubeba (may chang)
- Melissa officinalis (lemon balm)
- Myrtus communis (myrtle)
- Ocimum basilicum (basil)
- Origanum majorana (sweet marjoram)
- Ravensara aromatica (ravensara)
- Thymus vulgaris ct. geraniol, ct. linalool (sweet thyme)
- Valeriana officinalis (valerian)
How to Use Essential Oils for Anxiety
There are several natural therapies that can help quiet your mind and calm your anti-anxiety. Let's discuss some useful applications and essential oil combinations.
Diffusion – the easiest and arguably the most effective approach to use essential oils for anxiety is to put a few drops of any of these oils above (or a homemade blend) in your diffuser before you go to bed. Some nice diffuser blends you might want to try are:
- 2 drops ylang ylang, 1 drop bergamot, 1 drop lavender, 1 drop sweet marjoram, 1 drop roman chamomile and 1 drop valerian
- 2 drops lavender, 1 drop clary sage, 1 drop of ylang ylang and 1 drop vanilla
- 2 drops geranium, 1 drop sweet marjoram, 1 drop of patchouli and 1 drop sweet orange
- 2 drops roman chamomile, 1 drop rose and 1 drop palmarosa
Topical – another effective strategy is to simply apply these key oils over certain parts of the body – particularly the trigger points – like the bottoms of the feet, on the wrists, behind the knees, behind the ears on the mastoid bone or on the back of the neck.
Be sure to use with a good carrier oil, and creating a 2-3% dilution is considered safe by most experts. For example,
- 2% dilution: 12 drops of EO per oz of carrier oil (2% of 600 drops is 12)
If working with tablespoons is more comfortable for you, 1 oz. = 2 tablespoons. So, there are 300 drops of EO in a tablespoon.
- 2% dilution: 6 drops of EO per tablespoon of carrier oil (2% of 300 drops is 6)
Misting Spray – another great trick is to make a DIY Anxiety Spray. Using some of the same oils above:
- Add 20 drops of essential oils into a 4 oz glass spray bottle
- Fill the remaining bottle with water
- Shake well
Mist into the air and take in a deep breath during panic attacks, stressful moments or when anxiety settles in.
Other DIY Hacks – try making your favorite DIY recipes with these calming essential oils. It's a great way to calm the body and the mind. Here are some recipes for you – remember, just use the oils and blends above to give you the desired result:
- Detox bath
- Foaming hand soap
- Hand cream
- Hand sanitizer
- Healing skin serum
- Liquid hand soap
- Lotion bar
- Laundry detergent
- Sugar bath scrub
Safety & Contraindications
Are you sure you're using essential oils safely and effectively? Are you confused by dilutions and conversions?
Take out the guesswork and download FREE roller bottle guide HERE.
Additional Resources
- DeLeo D, Bertolote J, Lester, D. Self-directed violence. 2002. Chapter 7. In: Krug EG., Dahlberg LL., Mercy JA, Zwi A, Lozano R, eds. World report on violence and health[PDF 239 KB]. Geneva: World Health Organization.
- Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE, eds. Reducing suicide: a national imperative. Washington DC: National Academy Press; 2002.
- McLean, J, Maxwell, M, Platt, S, Harris, F, and Jepson, R. Risk and Protective Factors for Suicide and Suicidal Behaviour: a Literature Review. Scottish Government Social Research. Edinborough. 2008.
- U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention. National Strategy for Suicide Prevention: Goals and Objectives for Action. Washington DC: HHS; 2012.
- U.S. Public Health Service. The surgeon general’s call to action to prevent suicide. Washington DC: US Department of Health and Human Services; 1999.
- World Health Organization. Preventing suicide: A global imperative. Geneva, Switzerland: WHO; 2014.