Ankylosing Spondylitis
Questions and Answers about Ankylosing Spondylitis
This article contains general information about Ankylosing Spondylitis (AS). It describes what ankylosing spondylitis is, its causes, and treatment options. Highlights of current research are also included. At the end is a list of key words to help you understand the terms used in this article. If you have further questions, you may wish to discuss them with your health care provider.
Chances are that you have a really bad back and your doctor, not a Rheumatologist or Orthopedic doctor, your Primary Care doctor had matter-of-factly told you several times that you just have Arthritis in your back, knees, shoulder, neck or wherever the problem is manifested...and you believed that there is not much you can do about it, except suck it up and bear the constant, or intermittent pain. Saying it's arthritis is probably his way of explaining it, but did he send you for a consult with a Rheumatologist or Orthopedic specialist? Did you have the pertinent tests done to get you an informed diagnosis, so you could at least understand the prognosis?
Lets talk about about this arthritis in the back...we don't want you to think that every back pain is ankylosing Spondylitis...
Here's what I know based on my Orthopedic doctor's diagnosis, based on questioning, imaging results and labs.
What Is Ankylosing Spondylitis - AS?
Lower back pain is a common health problem. It is typically caused by injury or strain to the back, known as mechanical back pain. But your back pain could also be signaling a more serious condition.
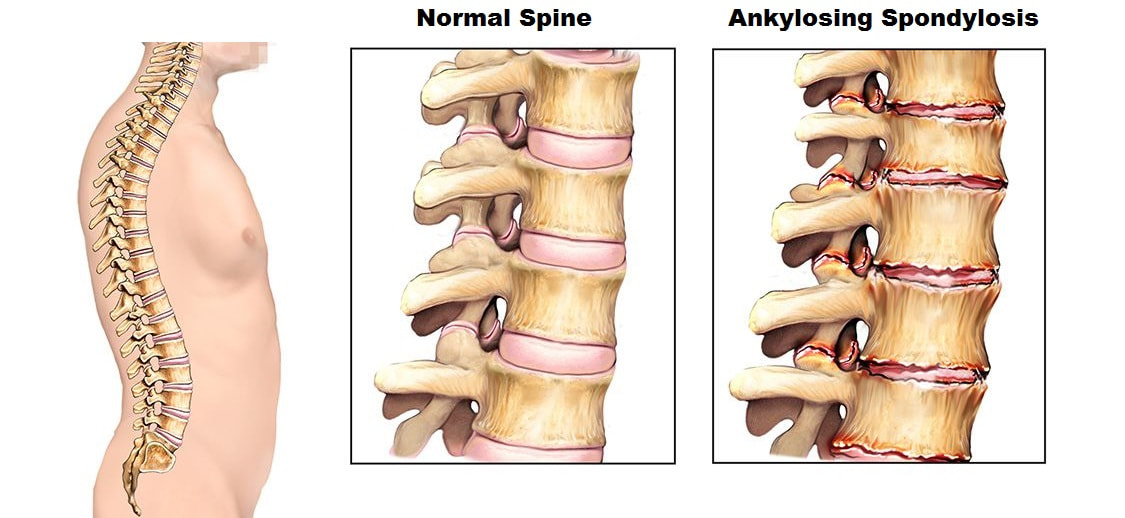
Ankylosing spondylitis - AS—pronounced ANK-ki-low-sing spon-di-LIE-tis--is a chronic, progressive, inflammatory disease of the joints in the spine. AS occurs when the immune system mistakenly attacks healthy joints, mainly in the spine. This immune response causes inflammation, which contributes to pain and stiffness in these joints. This is known as inflammatory back pain. Because AS is a chronic disease, there is no known cure, and the focus is on controlling symptoms. If left untreated, over time the pain and stiffness of AS can become persistent and can occur in other parts of the body.
So doctors refer to it as a form of progressive arthritis due to the chronic inflammation of the joints in the spine. Its name comes from the Greek words “ankylos,” meaning stiffening of a joint, and “spondylo,” meaning vertebra. Spondylitis refers to inflammation of the spine or one or more of the adjacent structures of the vertebrae.
Ankylosing spondylitis belongs to a group of disorders called seronegative spondyloarthropathies. Seronegative means an individual has tested negative for an autoantibody called rheumatoid factor. The spondyloarthropathies are a family of similar diseases that usually cause joint and spine inflammation. Other well-established syndromes in this group include psoriatic arthritis, the arthritis of inflammatory bowel disease, chronic reactive arthritis, and enthesitis-related idiopathic juvenile arthritis.
Although these disorders have similarities, they also have features that distinguish them from one another. The hallmark of ankylosing spondylitis is “sacroiliitis,” or inflammation of the sacroiliac (SI) joints, where the spine joins the pelvis.
In some people, ankylosing spondylitis can affect joints outside of the spine, like the shoulders, ribs, hips, knees, and feet. It can also affect entheses, which are sites where the tendons and ligaments attach to the bones. It is possible that it can affect other organs, such as the eyes, bowel, and—more rarely—the heart and lungs.
Although many people with ankylosing spondylitis have mild episodes of back pain that come and go, others have severe, ongoing pain accompanied by loss of flexibility of the spine. In the most severe cases, long-term inflammation leads to calcification that causes two or more bones of the spine to fuse. Fusion can also stiffen the rib cage, resulting in restricted lung capacity and function.
Who Has Ankylosing Spondylitis?
Ankylosing spondylitis typically begins in adolescents and young adults, but it affects people for the rest of their lives. Men are more likely to develop ankylosing spondylitis than are women. If your teenager or young adult child is complaining of bad back pain, knee pain or eye pain with redness, its time to get a good look at the reason for that problem. The earlier the problem gets managed, the most likely that the progression will be slowed and there will be better quality of life later on. Unfortunately, Ankylosing Spondylosis usually gets diagnosed much later in life.
What Causes Ankylosing Spondylitis?
The cause of ankylosing spondylitis is unknown, but it is likely that both genes and factors in the environment play a role. The main gene associated with susceptibility to ankylosing spondylitis is called HLA-B27. But while most people with ankylosing spondylitis have this genetic marker, only a small percentage of people with the gene develop the disease.
Signs and symptoms
Ankylosing spondylitis
Key components of the patient history that suggest AS include the following:
General symptoms of AS include the following:
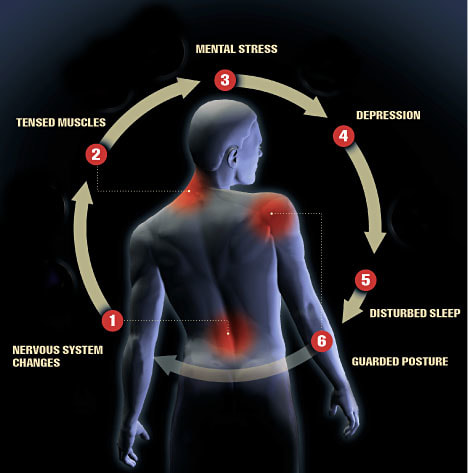
Fatigue is another common complaint, occurring in approximately 65% of patients with AS. Increased levels of fatigue are associated with increased pain and stiffness and decreased functional capacity. [2, 3]
Extra-articular manifestations of AS can include the following:
Undifferentiated spondyloarthropathy
Clinical manifestations of undifferentiated spondyloarthropathy include the following:
This article contains general information about Ankylosing Spondylitis (AS). It describes what ankylosing spondylitis is, its causes, and treatment options. Highlights of current research are also included. At the end is a list of key words to help you understand the terms used in this article. If you have further questions, you may wish to discuss them with your health care provider.
Chances are that you have a really bad back and your doctor, not a Rheumatologist or Orthopedic doctor, your Primary Care doctor had matter-of-factly told you several times that you just have Arthritis in your back, knees, shoulder, neck or wherever the problem is manifested...and you believed that there is not much you can do about it, except suck it up and bear the constant, or intermittent pain. Saying it's arthritis is probably his way of explaining it, but did he send you for a consult with a Rheumatologist or Orthopedic specialist? Did you have the pertinent tests done to get you an informed diagnosis, so you could at least understand the prognosis?
Lets talk about about this arthritis in the back...we don't want you to think that every back pain is ankylosing Spondylitis...
Here's what I know based on my Orthopedic doctor's diagnosis, based on questioning, imaging results and labs.
What Is Ankylosing Spondylitis - AS?
Lower back pain is a common health problem. It is typically caused by injury or strain to the back, known as mechanical back pain. But your back pain could also be signaling a more serious condition.
Ankylosing spondylitis - AS—pronounced ANK-ki-low-sing spon-di-LIE-tis--is a chronic, progressive, inflammatory disease of the joints in the spine. AS occurs when the immune system mistakenly attacks healthy joints, mainly in the spine. This immune response causes inflammation, which contributes to pain and stiffness in these joints. This is known as inflammatory back pain. Because AS is a chronic disease, there is no known cure, and the focus is on controlling symptoms. If left untreated, over time the pain and stiffness of AS can become persistent and can occur in other parts of the body.
So doctors refer to it as a form of progressive arthritis due to the chronic inflammation of the joints in the spine. Its name comes from the Greek words “ankylos,” meaning stiffening of a joint, and “spondylo,” meaning vertebra. Spondylitis refers to inflammation of the spine or one or more of the adjacent structures of the vertebrae.
Ankylosing spondylitis belongs to a group of disorders called seronegative spondyloarthropathies. Seronegative means an individual has tested negative for an autoantibody called rheumatoid factor. The spondyloarthropathies are a family of similar diseases that usually cause joint and spine inflammation. Other well-established syndromes in this group include psoriatic arthritis, the arthritis of inflammatory bowel disease, chronic reactive arthritis, and enthesitis-related idiopathic juvenile arthritis.
Although these disorders have similarities, they also have features that distinguish them from one another. The hallmark of ankylosing spondylitis is “sacroiliitis,” or inflammation of the sacroiliac (SI) joints, where the spine joins the pelvis.
In some people, ankylosing spondylitis can affect joints outside of the spine, like the shoulders, ribs, hips, knees, and feet. It can also affect entheses, which are sites where the tendons and ligaments attach to the bones. It is possible that it can affect other organs, such as the eyes, bowel, and—more rarely—the heart and lungs.
Although many people with ankylosing spondylitis have mild episodes of back pain that come and go, others have severe, ongoing pain accompanied by loss of flexibility of the spine. In the most severe cases, long-term inflammation leads to calcification that causes two or more bones of the spine to fuse. Fusion can also stiffen the rib cage, resulting in restricted lung capacity and function.
Who Has Ankylosing Spondylitis?
Ankylosing spondylitis typically begins in adolescents and young adults, but it affects people for the rest of their lives. Men are more likely to develop ankylosing spondylitis than are women. If your teenager or young adult child is complaining of bad back pain, knee pain or eye pain with redness, its time to get a good look at the reason for that problem. The earlier the problem gets managed, the most likely that the progression will be slowed and there will be better quality of life later on. Unfortunately, Ankylosing Spondylosis usually gets diagnosed much later in life.
What Causes Ankylosing Spondylitis?
The cause of ankylosing spondylitis is unknown, but it is likely that both genes and factors in the environment play a role. The main gene associated with susceptibility to ankylosing spondylitis is called HLA-B27. But while most people with ankylosing spondylitis have this genetic marker, only a small percentage of people with the gene develop the disease.
Signs and symptoms
Ankylosing spondylitis
Key components of the patient history that suggest AS include the following:
- Insidious onset of low back pain - The most common symptom
- Onset of symptoms before age 40 years
- Presence of symptoms for more than 3 months
- Symptoms worse in the morning or with inactivity
- Improvement of symptoms with exercise [1]
General symptoms of AS include the following:
- Those related to inflammatory back pain - Stiffness of the spine and kyphosis resulting in a stooped posture are characteristic of advanced-stage AS.
- Peripheral enthesitis and arthritis
- Constitutional and organ-specific extra-articular manifestations
Fatigue is another common complaint, occurring in approximately 65% of patients with AS. Increased levels of fatigue are associated with increased pain and stiffness and decreased functional capacity. [2, 3]
Extra-articular manifestations of AS can include the following:
- Uveitis
- Cardiovascular disease
- Pulmonary disease
- Renal disease
- Neurologic disease
- Gastrointestinal (GI) disease
- Metabolic bone disease
Undifferentiated spondyloarthropathy
Clinical manifestations of undifferentiated spondyloarthropathy include the following:
- Inflammatory back pain - 90%
- Buttock pain - 80%
- Enthesitis - 85%
- Peripheral arthritis - 35%
- Dactylitis - 17%
- Fatigue - 55%
How Is Ankylosing Spondylitis Diagnosed?
A diagnosis of ankylosing spondylitis is based largely on the findings of a medical history and physical exam. Radiologic tests and lab tests may be used to help confirm a diagnosis, but both have some limitations.
Medical History
The medical history involves answering questions, such as the following:
· How long have you had pain?
· Where specifically is the pain in your back or neck? Are other joints affected?
· Is back pain better with exercise and worse after inactivity, such as when you first get up in the morning?
· Do you have other problems, such as eye problems or fatigue?
· Does anyone in your family have back problems or arthritis?
· Have you recently suffered from a gastrointestinal illness?
· Do you have any skin rashes such as psoriasis?
From your answers to these questions, your doctor can begin to get an idea of the diagnosis.
Physical Exam
During the physical exam, the doctor will look for signs and symptoms that are consistent with ankylosing spondylitis. These include pain along the spine and/or in the pelvis, sacroiliac joints, heels, and chest. Your doctor may ask you to move and bend in different directions to check the flexibility of your spine and to breathe deeply to check for any problems with chest expansion, which could be caused by inflammation in the joints where the ribs attach to the spine.
Radiologic Tests
X rays and magnetic resonance imaging (MRI) may be used in making or confirming a diagnosis of ankylosing spondylitis, but these tests have limitations. X rays may show changes in the spine and sacroiliac joints that indicate ankylosing spondylitis; however, it may take years of inflammation to cause damage that is visible on x rays. MRI may allow for earlier diagnosis, because it can show damage to soft tissues and bone before it can be seen on an x ray. Both tests may also be used to monitor the progression of ankylosing spondylitis. Radiographic evidence of inflammatory changes in the SI joints and spine are useful in the diagnosis and ongoing evaluation of AS. [7]
Early radiographic signs of enthesitis include squaring of the vertebral bodies caused by erosions of the superior and inferior margins of these bodies, resulting in loss of the normal concave contour of the bodies’ anterior surface. The inflammatory lesions at vertebral entheses may result in sclerosis of the superior and inferior margins of the vertebral bodies, called shiny corners (Romanus lesion).
Power Doppler ultrasonography can be used to document active enthesitis. In addition, this technology may be useful in the assessment of changes in inflammatory activity at entheses during the institution of new therapies. [8]
MRI and CT scanning
Magnetic resonance imaging (MRI) or computed tomography (CT) scanning of the SI joints, spine, and peripheral joints may reveal evidence of early sacroiliitis, erosions, and enthesitis that are not apparent on standard radiographs. [9, 10]
Lab Tests
The main blood test for ankylosing spondylitis is one to check for the HLA-B27 gene, which is present in the majority of Caucasians with ankylosing spondylitis. However, this test also has limitations. The gene is found in much lower percentages of African Americans with ankylosing spondylitis, and in ankylosing spondylitis patients from some Mediterranean countries. Also, the gene is found in many people who do not have ankylosing spondylitis, and will never get it. Still, when the gene is found in people who have symptoms of ankylosing spondylitis and/or x-ray evidence of ankylosing spondylitis, this finding helps support the ankylosing spondylitis diagnosis.
What is C-reactive protein CRP?
C-reactive protein (CRP) is a blood test marker for inflammation in the body. CRP is produced in the liver and its level is measured by testing the blood. Other names for CRP are high-sensitivity C-reactive protein (hs-CRP) and ultra-sensitive C-reactive protein (us-CRP).
A high level of CRP in the blood is a marker of inflammation. It can be caused by a wide variety of conditions, from infection to cancer. High CRP levels can also indicate that there’s inflammation in the arteries of the heart, which can mean a higher risk for heart attack. Eye inflammation (redness and pain) occurs in some people with spondylitis. Knowing the level of inflammation is key to managing it.
What Type of Doctor Diagnoses and Treats Ankylosing Spondylitis?
The diagnosis of ankylosing spondylitis is often made by a rheumatologist, a doctor specially trained to diagnose and treat arthritis and related conditions of the musculoskeletal system. However, because ankylosing spondylitis can affect different parts of the body, a person with the disorder may need to see several different types of doctors for treatment. In addition to a rheumatologist, there are many different specialists who treat ankylosing spondylitis.
These may include:
· An ophthalmologist, who treats eye disease.
· A gastroenterologist, who treats bowel disease.
· A physiatrist, a medical doctor who specializes in physical medicine and rehabilitation.
· A physical therapist or rehabilitation specialist, who supervises stretching and exercise regimens.
Often, it is helpful to the doctors and the patient for one doctor to manage the complete treatment plan.
Can Ankylosing Spondylitis Be Cured?
There is no cure for ankylosing spondylitis, but some treatments relieve symptoms of the disorder and may possibly prevent its progression. In most cases, treatment involves a combination of medication, exercise, and self-help measures. In some cases, surgery may be used to repair some of the joint damage caused by the disease.
Conventional Treatments: What Medications Are Used to Treat Ankylosing Spondylitis?
Several classes of medications are used to treat ankylosing spondylitis. Because there are many medication options, it’s important to work with your doctor to find the safest and most effective treatment plan for you. A treatment plan for ankylosing spondylitis will likely include one or more of the following:1
Management
Pharmacologic therapy (Conventional Medicine)
Agents used in the treatment of AS include the following:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
These drugs relieve pain and inflammation, and are commonly used to treat ankylosing spondylitis. Aspirin, ibuprofen, and naproxen are examples of NSAIDs. All NSAIDs work similarly by blocking substances called prostaglandins that contribute to inflammation and pain. However, each NSAID is a different chemical, and each has a slightly different effect on the body.2
1. All medicines can have side effects.
Some medicines and side effects are mentioned in this publication. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your health care provider or pharmacist if you have any questions about the possible side effects.
2. Warning:
Side effects of NSAIDs include stomach problems; skin rashes; high blood pressure; fluid retention; and liver, kidney, and heart problems. The longer a person uses NSAIDs, the more likely he or she is to have side effects, ranging from mild to serious. Many other drugs cannot be taken when a patient is being treated with NSAIDs, because NSAIDs alter the way the body uses or eliminates these other drugs. Check with your health care provider or pharmacist before you take NSAIDs. NSAIDs should only be used at the lowest dose possible for the shortest time needed.
Some NSAIDs are available over the counter, but more than a dozen others, including a subclass called COX-2 inhibitors, are available only with a prescription.
All NSAIDs can have significant side effects, and for unknown reasons, some people seem to respond better to one NSAID than another. Anyone taking NSAIDs regularly should be monitored by a doctor.
Corticosteroids
These strong inflammation-fighting drugs are similar to the cortisone made by our bodies. If NSAIDs alone do not control inflammation in people with ankylosing spondylitis, doctors may inject corticosteroids directly into the affected joints to bring quick but temporary relief. Injections may be given to the sacroiliac joint, hip joint, or knee joint, but are not given in the spine.
Disease-Modifying Antirheumatic Drugs (DMARDs)
These drugs work in different ways to control the disease process of ankylosing spondylitis. The most commonly used DMARDs for ankylosing spondylitis are sulfasalazine and methotrexate.
Biologic Agents
Members of this class of medications are genetically engineered to block proteins involved in the body’s inflammatory response. Five biologics—adalimumab, certolizumab, etanercept, golimumab, and infliximab—are approved by the Food and Drug Administration (FDA) for treating ankylosing spondylitis. All four work by suppressing a protein called tumor necrosis factor-alpha (TNF-α), and are often effective for relieving symptoms when NSAIDs or other treatments are not. These drugs are taken by intravenous infusion or injection.
Will Diet and Exercise Help?
A healthy diet and exercise are good for everyone, but may be especially helpful if you have ankylosing spondylitis.
Exercise and stretching, when done carefully and increased gradually, may help painful, stiff joints.
Strengthening exercises, performed with weights or done by tightening muscles without moving the joints, build the muscles around painful joints to better support them. Exercises that don’t require joint movement can be done even when your joints are painful and inflamed.
Range-of-motion exercises improve movement and flexibility and reduce stiffness in the affected joint. If the spine is painful and/or inflamed, exercises to stretch and extend the back can be helpful in preventing long-term disability.
Many people with ankylosing spondylitis find it helpful to exercise in water.
Before beginning an exercise program, it’s important to speak with a health professional who can recommend appropriate exercises.
When Might Surgery Be Necessary, and How Can It Help?
Surgical therapy
The following procedures can be used in the surgical management of AS:
If ankylosing spondylitis causes severe joint damage that makes it difficult to do your daily activities, total joint replacement may be an option. This involves removing the damaged joint and replacing it with a prosthesis made of metals, plastics, and/or ceramic materials. The most commonly replaced joints are the knee and hip.
In very rare cases, a procedure called osteotomy may be used to straighten a spine that has fused into a curved-forward position. This surgery involves cutting through the spine so that it can be realigned to a more vertical position. After the bones are realigned, hardware may be implanted to hold them in their new position while the spine heals.
Surgery to straighten the spine can only be done by a surgeon with significant experience in the procedure. Many doctors and surgeons consider the procedure high risk.
What Are Some Things I Can Do to Help Myself?
Aside from seeing your doctor regularly and following your prescribed treatment plan, staying active is probably the best thing you can do for ankylosing spondylitis. Regular exercise can help relieve pain, improve posture, and maintain flexibility. Before beginning an exercise program, speak with your doctor or physical therapist about designing a program that’s right for you.
Another important thing you can do for yourself is to practice good posture. A good test for posture is to check yourself in a mirror. First, stand with a full-length mirror to your side and, if possible, turn your head to look at your profile. Next, imagine you have dropped a weighted string from the top of your head to the soles of your feet. Where does the string fall?
If your posture is good, it should pass through your earlobe, the front of your shoulder, the center of your hip, behind your kneecap, and in front of your anklebone. If you are not standing that way already, practice holding your body that way in front of a mirror until you know well how it feels. Practicing good posture can help you avoid some of the complications that can occur with ankylosing spondylitis.
A diagnosis of ankylosing spondylitis is based largely on the findings of a medical history and physical exam. Radiologic tests and lab tests may be used to help confirm a diagnosis, but both have some limitations.
Medical History
The medical history involves answering questions, such as the following:
· How long have you had pain?
· Where specifically is the pain in your back or neck? Are other joints affected?
· Is back pain better with exercise and worse after inactivity, such as when you first get up in the morning?
· Do you have other problems, such as eye problems or fatigue?
· Does anyone in your family have back problems or arthritis?
· Have you recently suffered from a gastrointestinal illness?
· Do you have any skin rashes such as psoriasis?
From your answers to these questions, your doctor can begin to get an idea of the diagnosis.
Physical Exam
During the physical exam, the doctor will look for signs and symptoms that are consistent with ankylosing spondylitis. These include pain along the spine and/or in the pelvis, sacroiliac joints, heels, and chest. Your doctor may ask you to move and bend in different directions to check the flexibility of your spine and to breathe deeply to check for any problems with chest expansion, which could be caused by inflammation in the joints where the ribs attach to the spine.
Radiologic Tests
X rays and magnetic resonance imaging (MRI) may be used in making or confirming a diagnosis of ankylosing spondylitis, but these tests have limitations. X rays may show changes in the spine and sacroiliac joints that indicate ankylosing spondylitis; however, it may take years of inflammation to cause damage that is visible on x rays. MRI may allow for earlier diagnosis, because it can show damage to soft tissues and bone before it can be seen on an x ray. Both tests may also be used to monitor the progression of ankylosing spondylitis. Radiographic evidence of inflammatory changes in the SI joints and spine are useful in the diagnosis and ongoing evaluation of AS. [7]
Early radiographic signs of enthesitis include squaring of the vertebral bodies caused by erosions of the superior and inferior margins of these bodies, resulting in loss of the normal concave contour of the bodies’ anterior surface. The inflammatory lesions at vertebral entheses may result in sclerosis of the superior and inferior margins of the vertebral bodies, called shiny corners (Romanus lesion).
Power Doppler ultrasonography can be used to document active enthesitis. In addition, this technology may be useful in the assessment of changes in inflammatory activity at entheses during the institution of new therapies. [8]
MRI and CT scanning
Magnetic resonance imaging (MRI) or computed tomography (CT) scanning of the SI joints, spine, and peripheral joints may reveal evidence of early sacroiliitis, erosions, and enthesitis that are not apparent on standard radiographs. [9, 10]
Lab Tests
The main blood test for ankylosing spondylitis is one to check for the HLA-B27 gene, which is present in the majority of Caucasians with ankylosing spondylitis. However, this test also has limitations. The gene is found in much lower percentages of African Americans with ankylosing spondylitis, and in ankylosing spondylitis patients from some Mediterranean countries. Also, the gene is found in many people who do not have ankylosing spondylitis, and will never get it. Still, when the gene is found in people who have symptoms of ankylosing spondylitis and/or x-ray evidence of ankylosing spondylitis, this finding helps support the ankylosing spondylitis diagnosis.
What is C-reactive protein CRP?
C-reactive protein (CRP) is a blood test marker for inflammation in the body. CRP is produced in the liver and its level is measured by testing the blood. Other names for CRP are high-sensitivity C-reactive protein (hs-CRP) and ultra-sensitive C-reactive protein (us-CRP).
A high level of CRP in the blood is a marker of inflammation. It can be caused by a wide variety of conditions, from infection to cancer. High CRP levels can also indicate that there’s inflammation in the arteries of the heart, which can mean a higher risk for heart attack. Eye inflammation (redness and pain) occurs in some people with spondylitis. Knowing the level of inflammation is key to managing it.
What Type of Doctor Diagnoses and Treats Ankylosing Spondylitis?
The diagnosis of ankylosing spondylitis is often made by a rheumatologist, a doctor specially trained to diagnose and treat arthritis and related conditions of the musculoskeletal system. However, because ankylosing spondylitis can affect different parts of the body, a person with the disorder may need to see several different types of doctors for treatment. In addition to a rheumatologist, there are many different specialists who treat ankylosing spondylitis.
These may include:
· An ophthalmologist, who treats eye disease.
· A gastroenterologist, who treats bowel disease.
· A physiatrist, a medical doctor who specializes in physical medicine and rehabilitation.
· A physical therapist or rehabilitation specialist, who supervises stretching and exercise regimens.
Often, it is helpful to the doctors and the patient for one doctor to manage the complete treatment plan.
Can Ankylosing Spondylitis Be Cured?
There is no cure for ankylosing spondylitis, but some treatments relieve symptoms of the disorder and may possibly prevent its progression. In most cases, treatment involves a combination of medication, exercise, and self-help measures. In some cases, surgery may be used to repair some of the joint damage caused by the disease.
Conventional Treatments: What Medications Are Used to Treat Ankylosing Spondylitis?
Several classes of medications are used to treat ankylosing spondylitis. Because there are many medication options, it’s important to work with your doctor to find the safest and most effective treatment plan for you. A treatment plan for ankylosing spondylitis will likely include one or more of the following:1
Management
Pharmacologic therapy (Conventional Medicine)
Agents used in the treatment of AS include the following:
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Sulfasalazine
- Tumor necrosis factor-α (TNF-α) antagonists
- Corticosteroids
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
These drugs relieve pain and inflammation, and are commonly used to treat ankylosing spondylitis. Aspirin, ibuprofen, and naproxen are examples of NSAIDs. All NSAIDs work similarly by blocking substances called prostaglandins that contribute to inflammation and pain. However, each NSAID is a different chemical, and each has a slightly different effect on the body.2
1. All medicines can have side effects.
Some medicines and side effects are mentioned in this publication. Some side effects may be more severe than others. You should review the package insert that comes with your medicine and ask your health care provider or pharmacist if you have any questions about the possible side effects.
2. Warning:
Side effects of NSAIDs include stomach problems; skin rashes; high blood pressure; fluid retention; and liver, kidney, and heart problems. The longer a person uses NSAIDs, the more likely he or she is to have side effects, ranging from mild to serious. Many other drugs cannot be taken when a patient is being treated with NSAIDs, because NSAIDs alter the way the body uses or eliminates these other drugs. Check with your health care provider or pharmacist before you take NSAIDs. NSAIDs should only be used at the lowest dose possible for the shortest time needed.
Some NSAIDs are available over the counter, but more than a dozen others, including a subclass called COX-2 inhibitors, are available only with a prescription.
All NSAIDs can have significant side effects, and for unknown reasons, some people seem to respond better to one NSAID than another. Anyone taking NSAIDs regularly should be monitored by a doctor.
Corticosteroids
These strong inflammation-fighting drugs are similar to the cortisone made by our bodies. If NSAIDs alone do not control inflammation in people with ankylosing spondylitis, doctors may inject corticosteroids directly into the affected joints to bring quick but temporary relief. Injections may be given to the sacroiliac joint, hip joint, or knee joint, but are not given in the spine.
Disease-Modifying Antirheumatic Drugs (DMARDs)
These drugs work in different ways to control the disease process of ankylosing spondylitis. The most commonly used DMARDs for ankylosing spondylitis are sulfasalazine and methotrexate.
Biologic Agents
Members of this class of medications are genetically engineered to block proteins involved in the body’s inflammatory response. Five biologics—adalimumab, certolizumab, etanercept, golimumab, and infliximab—are approved by the Food and Drug Administration (FDA) for treating ankylosing spondylitis. All four work by suppressing a protein called tumor necrosis factor-alpha (TNF-α), and are often effective for relieving symptoms when NSAIDs or other treatments are not. These drugs are taken by intravenous infusion or injection.
Will Diet and Exercise Help?
A healthy diet and exercise are good for everyone, but may be especially helpful if you have ankylosing spondylitis.
Exercise and stretching, when done carefully and increased gradually, may help painful, stiff joints.
Strengthening exercises, performed with weights or done by tightening muscles without moving the joints, build the muscles around painful joints to better support them. Exercises that don’t require joint movement can be done even when your joints are painful and inflamed.
Range-of-motion exercises improve movement and flexibility and reduce stiffness in the affected joint. If the spine is painful and/or inflamed, exercises to stretch and extend the back can be helpful in preventing long-term disability.
Many people with ankylosing spondylitis find it helpful to exercise in water.
Before beginning an exercise program, it’s important to speak with a health professional who can recommend appropriate exercises.
When Might Surgery Be Necessary, and How Can It Help?
Surgical therapy
The following procedures can be used in the surgical management of AS:
- Vertebral osteotomy - Patients with fusion of the cervical or upper thoracic spine may benefit from extension osteotomy of the cervical spine [11]
- Fracture stabilization
- Joint replacement - Patients with significant involvement of the hips may benefit from total hip arthroplasty [12]
If ankylosing spondylitis causes severe joint damage that makes it difficult to do your daily activities, total joint replacement may be an option. This involves removing the damaged joint and replacing it with a prosthesis made of metals, plastics, and/or ceramic materials. The most commonly replaced joints are the knee and hip.
In very rare cases, a procedure called osteotomy may be used to straighten a spine that has fused into a curved-forward position. This surgery involves cutting through the spine so that it can be realigned to a more vertical position. After the bones are realigned, hardware may be implanted to hold them in their new position while the spine heals.
Surgery to straighten the spine can only be done by a surgeon with significant experience in the procedure. Many doctors and surgeons consider the procedure high risk.
What Are Some Things I Can Do to Help Myself?
Aside from seeing your doctor regularly and following your prescribed treatment plan, staying active is probably the best thing you can do for ankylosing spondylitis. Regular exercise can help relieve pain, improve posture, and maintain flexibility. Before beginning an exercise program, speak with your doctor or physical therapist about designing a program that’s right for you.
Another important thing you can do for yourself is to practice good posture. A good test for posture is to check yourself in a mirror. First, stand with a full-length mirror to your side and, if possible, turn your head to look at your profile. Next, imagine you have dropped a weighted string from the top of your head to the soles of your feet. Where does the string fall?
If your posture is good, it should pass through your earlobe, the front of your shoulder, the center of your hip, behind your kneecap, and in front of your anklebone. If you are not standing that way already, practice holding your body that way in front of a mirror until you know well how it feels. Practicing good posture can help you avoid some of the complications that can occur with ankylosing spondylitis.
Alternative Treatments for Ankylosing Spondylitis
Alternative treatments or home remedies that have been listed as possibly helpful for Ankylosing Spondylitis may include:
Natural Ways to Relieve Ankylosing Spondylitis Pain
Managing ankylosing spondylitis means controlling symptoms like morning stiffness and back pain. Try these strategies for natural pain relief.
One of the most frustrating things about ankylosing spondylitis is experiencing pain not from exertion but from doing nothing more than trying to get a good night's sleep.
Back pain — the most common symptom of ankylosing spondylitis — and stiffness get worse with rest, so they're probably at their worst in the morning, just when you want to get your day started. You might also have pain and stiffness in other areas of your body, such as your neck, shoulders, hips, or feet.
While it's important to work with your doctor to find the best medications for ankylosing spondylitis, there are also some natural pain-relief strategies to help manage back pain and other symptoms, and you can use many of them every day: Alternative treatments, complementary therapeutic options, or home remedies that have been listed in various sources as possibly helpful for Ankylosing Spondylitis may include:
1. Exercise and stretching. “If you have ankylosing spondylitis, you need to stay active to maintain your flexibility," says Rochella Ostrowski, MD, an associate professor in the division of allergy, immunology, and rheumatology at Loyola Medicine in Maywood, Illinois. "The best exercises are those that avoid high impact." She suggests working with a physical therapist to get started. A physical therapist can design the right exercise and stretching program for you, including when to work out. Later in the day when you're less stiff may be the best time.
2. Good posture. “Check your posture frequently at home and at work," Dr. Ostrowski says. "Make sure you’re well-aligned and that you do gentle range-of-motion exercises often to avoid long periods of immobility." Reinforce good posture by regularly checking your alignment against a wall. You don’t want your spine to stiffen into a bent position, so aim for tall and straight.
3. Good posture in bed. “Sleep posture is also important," Ostrowski says. "You need a firm bed and a pillow that supports your neck properly. Avoid a pillow that’s too high. Sleeping on your belly is best for your posture, but some people can only sleep on their side or back.” If you're in that group, try spending a few minutes of your awake time practicing “prone lying”. This involves lying face down on a firm surface. For comfort, you can turn your head from side to side. This exercise helps promote better daily posture. Work up to 20-minute sessions to help with back pain relief.
4. Warm soaks. “A warm bath or shower is a natural way to relieve the pain and stiffness of ankylosing spondylitis," Ostrowski says. "Stretching to relieve pain and stiffness is also better after a warm shower. You should avoid stretching with cold joints and muscles." Alternating hot and cold compresses on painful spots is another natural pain-relief strategy you can try.
5. Acupuncture. This ancient technique that involves inserting thin needles through the skin may stimulate your body’s natural pain relievers. “Studies on acupuncture for back pain relief have had mixed results," Ostrowski says. "I don’t discourage it, and it’s helped some people with back pain.” One positive finding was published in December 2015 in the German journal Complementary Medicine Research. This research determined that acupuncture may be helpful in managing ankylosing spondylitis pain. Acupuncture should be performed by a trained and licensed acupuncture professional.
6. Massage. “Massage therapy, when performed by a therapist accustomed to working with ankylosing spondylitis, may be helpful,” Ostrowski says. Massage may not only help relieve the pain and stiffness of ankylosing spondylitis but also help ease the stress commonly brought on by having a chronic condition.
7. Yoga. “Yoga is a great natural pain reliever for ankylosing spondylitis,” Ostrowski says. "You need to start with very basic poses and be patient, but if you work with an instructor who can modify the yoga positions for you, you can really benefit from this form of exercise." A review of studies published in January 2016 in the Journal of Orthopedics & Rheumatology examined the impact of yoga on low back pain and found that it was safe and can help reduce both disability and pain.
8. Transcutaneous electrical nerve stimulation (TENS): TENS involves passing an electric current through the skin. It may work on the same principle as acupuncture — by bringing about the release of the body’s natural pain relievers. Although there have been some studies on TENS for back pain, results are mixed. Ostrowski says physical therapists may use TENS for pain that’s not responding to exercise and stretching.
9. Salba seeds and salba seed oil
An excellent plant source of omega-3 fatty acids.** They promote overall cardiovascular wellness and assist in the maintenance of proper blood sugar levels.**
Additionally, Salba Seeds:
· Supply fiber that promotes healthy digestion.**
· Supply antioxidants that fight oxidative stress.**
· May help to promote healthy weight management.**
10. Core strengthening exercise
11. Methylsulfonylmethane (MSM)
MSM (Methylsulfonylmethane) is an organic sulfur compound found naturally in the body which supports the creation of vital proteins and amino acids. It works to:
· Nourishe ligaments, cartilage & connective tissues.**
· Help to promote peak joint flexibility & comfort.**
· Support healthy & beautiful hair, skin and nails.**
12. Bromelain
Bromelain is a digestive enzyme derived from pineapple. It aids in maintaining healthy digestion and helps the body absorb proteins.** It can also:
· Modulate inflammatory responses.**
· Pptimize clear, comfortable sinuses.**
· Support healthy skin and joints.**
13. Valerian
Valerian soothes the central nervous system, accelerating the onset of sleep and promoting deep and restful slumber.** In addition, valerian may:
· Support feelings of relaxed tranquility.**
· Help to support relaxed muscles.**
· Help with nervousness and stress.**
14. Glucosamine sulfate
Glucosamine/Chondroitin supports joint health, delivering peak flexibility and mobility. A popular joint product, it works to soothe away aches and discomfort as well as:**
· Rejuvenates healthy cartilage.**
· Optimizes joint lubrication.**
· Nourishes and supports connective tissues.**
15. Chondroitin sulfate
Naturally found in in many parts of the body, chondroitin sulfate is a vital part of the structure and function of the cartilage found in joints.** As a supplement, chondroitin sulfate:
· Promotes joint health and mobility.**
· Helps support the elasticity and comfort of joint tissues.**
· Is often paired with other joint-supportive nutrients such as glucosamine.**
16. S-adenosyl-L-methionine (SAMe)
SAM-e is known for supporting emotional balance and maintaining a bright, positive mood. In addition to encouraging healthy aging and quality of life, SAM-e can:**
· Promote joint comfort and mobility.**
· Help rejuvenate cartilage.**
· Optimize nervous system and liver health.**
17. Curcumin/Turmeric
More than just a kitchen spice, turmeric—and its main compound curcumin—have long held an important place in herbal wellness traditions. Turmeric/Curcumin supplements:
· Deliver plant-based antioxidants known as curcuminoids.
· Support free radical-fighting antioxidant activity.**
· Are available in standardized forms and enhanced with black pepper extract.
18. Ginger
Ginger, a potent spice, has plentiful wellness benefits. Most noteably, ginger helps ease nausea, motion sickness and indigestion by promoting digestive wellness and comfort.** Its unique inflammaion-modulating properties help ginger to:
· Encourage free and easy mobility.**
· Optimize joint comfort.**
· Promote heart health and circulation.**
19. Mahanarayan oil
20. Guggul
Guggul is a longstanding part of Ayurvedic wellness traditions, used throughout India for thousands of years. This resin extract:
· Contains beneficial compounds known as guggulsterones.
· May help support healthy cholesterol levels already within normal range.**
· Delivers naturally-occurring antioxidant activity.**
21. Omega-3 fatty acids
Fish Oil supplies omega-3 fatty acids ALA, EPA and DHA. It also promotes cardiovascular wellness, immune system health, as well as:**
· Optimizing brain health, memory and mood.**
· Supporting peak bone mineral density.**
· Helping to support joint comfort and flexibility.**
22. LNA (alpha-linolenic acid)
Flax and flaxseed (linseed) oil promote overall wellness. Rich in omega-3 and omega-6 fatty acids, it is the best vegan source of omega-3 fatty acids. Flaxseed Oil is also known for:
· Supporting cardiovascular health.**
· Promoting women's health and hormonal balance.**
· Supporting men’s prostate and reproductive health.**
23. EPA (eicosapentaenoic acid)
Fish Oil supplies omega-3 fatty acids ALA, EPA and DHA. It also promotes cardiovascular wellness, immune system health, as well as:**
· Optimizing brain health, memory and mood.**
· Supporting peak bone mineral density.**
· Helping to support joint comfort and flexibility.**
24. DHA (docosahexaenoic acid)
DHA is an essential Omega-3 fatty acid found in fish oils. It promotes healthy brain, eye and nerve development and helps maintain concentration, focus and memory.** In addition, DHA works to:
· Support a bright, healthy mood.**
· Support heart, circulatory and cardiovascular health.**
· Optimize joint flexibility, mobility and comfort.**
25. GLA (gamma-linolenic acid)
Evening Primrose Oil contains omega-6 fatty acids, including GLA. It is a prized menopause support supplement and works to soothe away PMS and menstrual discomfort.** Evening Primrose Oil works to:
· Promote smooth, clear and healthy skin.**
· Modulate inflammatory responses.**
· Support joint and cardiovascular wellness.**
26. Evening primrose oil
Evening Primrose Oil contains omega-6 fatty acids, including GLA. It is a prized menopause support supplement and works to soothe away PMS and menstrual discomfort.** Evening Primrose Oil works to:
· Promote smooth, clear and healthy skin.**
· Modulate inflammatory responses.**
· Support joint and cardiovascular wellness.**
27. Avoid hydrogenated oils
28. Acupressure
Accupressure is the treatment whereby the body is pressed or massaged at the same locations as used in acupuncture. The application of pressure or localized massage to specific sites on the body to control symptoms such as pain or nausea.
29. Hara breathing
30. Mind-body exercise
31. Relaxation
32. Diet low in saturated fat
33. Fish
Fish Oil supplies omega-3 fatty acids ALA, EPA and DHA. It also promotes cardiovascular wellness, immune system health, as well as:**
· Optimizing brain health, memory and mood.**
· Supporting peak bone mineral density.**
· Helping to support joint comfort and flexibility.**
34. Unprocessed food
35. Avoid caffeine
36. Avoid alcohol
37. Avoid refined sugar
38. Avoid table salt
39. Olive oil
40. Juniper, lavender, cypress and rosemary oil in Epsom salt bath
41. Lavender and cypress oil in Epsom salt bath
42. Ginger chicken soup http://www.nourishingmeals.com/2011/02/healing-chicken-ginger-soup.html
Ayurvedic cleansing program (panchakarma)
Ginger tea with castor oil-by mouth
Simhanada guggulu-by mouth
Chitrak, and adhivati supplement-by mouth
Kaishore guggulu-by mouth
Cool castor oil
Cool coconut oil
Coconut Oil promotes optimal energy levels and supplies beneficial medium-chain triglycerides. It also promotes smoothe, supple skin in addition to:**
· Helping maintain the immune system.**
· Optimizing healthy metabolism.**
· Supporting weight management.**
Sandalwood Paste:
One of the most prized essential oils in aromatherapy, sandalwood oil is steam distilled from the fragrant wood of the East Indian sandalwood tree. In aromatherapy, this oil:
· Gently instills a sense of tranquility.
· Is a popular soothing meditative aid.
· Helps with quiet contemplation.
Ayurvedic dietary changes
Yoga
Breathing exercises
Amalaki tea
Other Tips for Ankylosing Spondylitis Pain Relief
Considering chiropractics?
Chiropractic treatment generally is NOT recommended for ankylosing spondylitis. “Chiropractic care isn’t advised for this type of back pain because changes from ankylosing spondylitis may increase the risk of injury during manipulation,” Ostrowski says. But there are a few other small steps you can take to help manage ankylosing spondylitis pain naturally. “I also recommend lots of deep breathing to keep your rib cage flexible, and I strongly advise against smoking," Ostrowski says. "Avoid physical and emotional stress as much as possible, have a good support system, and make sure to get enough rest.
"Sometimes with ankylosing spondylitis," she says, "you just need to take life a little slower.”
Alternative Treatments for Ankylosing Spondylitis
Alternative treatments or home remedies that have been listed as possibly helpful for Ankylosing Spondylitis may include:
Natural Ways to Relieve Ankylosing Spondylitis Pain
Managing ankylosing spondylitis means controlling symptoms like morning stiffness and back pain. Try these strategies for natural pain relief.
One of the most frustrating things about ankylosing spondylitis is experiencing pain not from exertion but from doing nothing more than trying to get a good night's sleep.
Back pain — the most common symptom of ankylosing spondylitis — and stiffness get worse with rest, so they're probably at their worst in the morning, just when you want to get your day started. You might also have pain and stiffness in other areas of your body, such as your neck, shoulders, hips, or feet.
While it's important to work with your doctor to find the best medications for ankylosing spondylitis, there are also some natural pain-relief strategies to help manage back pain and other symptoms, and you can use many of them every day: Alternative treatments, complementary therapeutic options, or home remedies that have been listed in various sources as possibly helpful for Ankylosing Spondylitis may include:
1. Exercise and stretching. “If you have ankylosing spondylitis, you need to stay active to maintain your flexibility," says Rochella Ostrowski, MD, an associate professor in the division of allergy, immunology, and rheumatology at Loyola Medicine in Maywood, Illinois. "The best exercises are those that avoid high impact." She suggests working with a physical therapist to get started. A physical therapist can design the right exercise and stretching program for you, including when to work out. Later in the day when you're less stiff may be the best time.
2. Good posture. “Check your posture frequently at home and at work," Dr. Ostrowski says. "Make sure you’re well-aligned and that you do gentle range-of-motion exercises often to avoid long periods of immobility." Reinforce good posture by regularly checking your alignment against a wall. You don’t want your spine to stiffen into a bent position, so aim for tall and straight.
3. Good posture in bed. “Sleep posture is also important," Ostrowski says. "You need a firm bed and a pillow that supports your neck properly. Avoid a pillow that’s too high. Sleeping on your belly is best for your posture, but some people can only sleep on their side or back.” If you're in that group, try spending a few minutes of your awake time practicing “prone lying”. This involves lying face down on a firm surface. For comfort, you can turn your head from side to side. This exercise helps promote better daily posture. Work up to 20-minute sessions to help with back pain relief.
4. Warm soaks. “A warm bath or shower is a natural way to relieve the pain and stiffness of ankylosing spondylitis," Ostrowski says. "Stretching to relieve pain and stiffness is also better after a warm shower. You should avoid stretching with cold joints and muscles." Alternating hot and cold compresses on painful spots is another natural pain-relief strategy you can try.
5. Acupuncture. This ancient technique that involves inserting thin needles through the skin may stimulate your body’s natural pain relievers. “Studies on acupuncture for back pain relief have had mixed results," Ostrowski says. "I don’t discourage it, and it’s helped some people with back pain.” One positive finding was published in December 2015 in the German journal Complementary Medicine Research. This research determined that acupuncture may be helpful in managing ankylosing spondylitis pain. Acupuncture should be performed by a trained and licensed acupuncture professional.
6. Massage. “Massage therapy, when performed by a therapist accustomed to working with ankylosing spondylitis, may be helpful,” Ostrowski says. Massage may not only help relieve the pain and stiffness of ankylosing spondylitis but also help ease the stress commonly brought on by having a chronic condition.
7. Yoga. “Yoga is a great natural pain reliever for ankylosing spondylitis,” Ostrowski says. "You need to start with very basic poses and be patient, but if you work with an instructor who can modify the yoga positions for you, you can really benefit from this form of exercise." A review of studies published in January 2016 in the Journal of Orthopedics & Rheumatology examined the impact of yoga on low back pain and found that it was safe and can help reduce both disability and pain.
8. Transcutaneous electrical nerve stimulation (TENS): TENS involves passing an electric current through the skin. It may work on the same principle as acupuncture — by bringing about the release of the body’s natural pain relievers. Although there have been some studies on TENS for back pain, results are mixed. Ostrowski says physical therapists may use TENS for pain that’s not responding to exercise and stretching.
9. Salba seeds and salba seed oil
An excellent plant source of omega-3 fatty acids.** They promote overall cardiovascular wellness and assist in the maintenance of proper blood sugar levels.**
Additionally, Salba Seeds:
· Supply fiber that promotes healthy digestion.**
· Supply antioxidants that fight oxidative stress.**
· May help to promote healthy weight management.**
10. Core strengthening exercise
11. Methylsulfonylmethane (MSM)
MSM (Methylsulfonylmethane) is an organic sulfur compound found naturally in the body which supports the creation of vital proteins and amino acids. It works to:
· Nourishe ligaments, cartilage & connective tissues.**
· Help to promote peak joint flexibility & comfort.**
· Support healthy & beautiful hair, skin and nails.**
12. Bromelain
Bromelain is a digestive enzyme derived from pineapple. It aids in maintaining healthy digestion and helps the body absorb proteins.** It can also:
· Modulate inflammatory responses.**
· Pptimize clear, comfortable sinuses.**
· Support healthy skin and joints.**
13. Valerian
Valerian soothes the central nervous system, accelerating the onset of sleep and promoting deep and restful slumber.** In addition, valerian may:
· Support feelings of relaxed tranquility.**
· Help to support relaxed muscles.**
· Help with nervousness and stress.**
14. Glucosamine sulfate
Glucosamine/Chondroitin supports joint health, delivering peak flexibility and mobility. A popular joint product, it works to soothe away aches and discomfort as well as:**
· Rejuvenates healthy cartilage.**
· Optimizes joint lubrication.**
· Nourishes and supports connective tissues.**
15. Chondroitin sulfate
Naturally found in in many parts of the body, chondroitin sulfate is a vital part of the structure and function of the cartilage found in joints.** As a supplement, chondroitin sulfate:
· Promotes joint health and mobility.**
· Helps support the elasticity and comfort of joint tissues.**
· Is often paired with other joint-supportive nutrients such as glucosamine.**
16. S-adenosyl-L-methionine (SAMe)
SAM-e is known for supporting emotional balance and maintaining a bright, positive mood. In addition to encouraging healthy aging and quality of life, SAM-e can:**
· Promote joint comfort and mobility.**
· Help rejuvenate cartilage.**
· Optimize nervous system and liver health.**
17. Curcumin/Turmeric
More than just a kitchen spice, turmeric—and its main compound curcumin—have long held an important place in herbal wellness traditions. Turmeric/Curcumin supplements:
· Deliver plant-based antioxidants known as curcuminoids.
· Support free radical-fighting antioxidant activity.**
· Are available in standardized forms and enhanced with black pepper extract.
18. Ginger
Ginger, a potent spice, has plentiful wellness benefits. Most noteably, ginger helps ease nausea, motion sickness and indigestion by promoting digestive wellness and comfort.** Its unique inflammaion-modulating properties help ginger to:
· Encourage free and easy mobility.**
· Optimize joint comfort.**
· Promote heart health and circulation.**
19. Mahanarayan oil
20. Guggul
Guggul is a longstanding part of Ayurvedic wellness traditions, used throughout India for thousands of years. This resin extract:
· Contains beneficial compounds known as guggulsterones.
· May help support healthy cholesterol levels already within normal range.**
· Delivers naturally-occurring antioxidant activity.**
21. Omega-3 fatty acids
Fish Oil supplies omega-3 fatty acids ALA, EPA and DHA. It also promotes cardiovascular wellness, immune system health, as well as:**
· Optimizing brain health, memory and mood.**
· Supporting peak bone mineral density.**
· Helping to support joint comfort and flexibility.**
22. LNA (alpha-linolenic acid)
Flax and flaxseed (linseed) oil promote overall wellness. Rich in omega-3 and omega-6 fatty acids, it is the best vegan source of omega-3 fatty acids. Flaxseed Oil is also known for:
· Supporting cardiovascular health.**
· Promoting women's health and hormonal balance.**
· Supporting men’s prostate and reproductive health.**
23. EPA (eicosapentaenoic acid)
Fish Oil supplies omega-3 fatty acids ALA, EPA and DHA. It also promotes cardiovascular wellness, immune system health, as well as:**
· Optimizing brain health, memory and mood.**
· Supporting peak bone mineral density.**
· Helping to support joint comfort and flexibility.**
24. DHA (docosahexaenoic acid)
DHA is an essential Omega-3 fatty acid found in fish oils. It promotes healthy brain, eye and nerve development and helps maintain concentration, focus and memory.** In addition, DHA works to:
· Support a bright, healthy mood.**
· Support heart, circulatory and cardiovascular health.**
· Optimize joint flexibility, mobility and comfort.**
25. GLA (gamma-linolenic acid)
Evening Primrose Oil contains omega-6 fatty acids, including GLA. It is a prized menopause support supplement and works to soothe away PMS and menstrual discomfort.** Evening Primrose Oil works to:
· Promote smooth, clear and healthy skin.**
· Modulate inflammatory responses.**
· Support joint and cardiovascular wellness.**
26. Evening primrose oil
Evening Primrose Oil contains omega-6 fatty acids, including GLA. It is a prized menopause support supplement and works to soothe away PMS and menstrual discomfort.** Evening Primrose Oil works to:
· Promote smooth, clear and healthy skin.**
· Modulate inflammatory responses.**
· Support joint and cardiovascular wellness.**
27. Avoid hydrogenated oils
28. Acupressure
Accupressure is the treatment whereby the body is pressed or massaged at the same locations as used in acupuncture. The application of pressure or localized massage to specific sites on the body to control symptoms such as pain or nausea.
29. Hara breathing
30. Mind-body exercise
31. Relaxation
32. Diet low in saturated fat
33. Fish
Fish Oil supplies omega-3 fatty acids ALA, EPA and DHA. It also promotes cardiovascular wellness, immune system health, as well as:**
· Optimizing brain health, memory and mood.**
· Supporting peak bone mineral density.**
· Helping to support joint comfort and flexibility.**
34. Unprocessed food
35. Avoid caffeine
36. Avoid alcohol
37. Avoid refined sugar
38. Avoid table salt
39. Olive oil
40. Juniper, lavender, cypress and rosemary oil in Epsom salt bath
41. Lavender and cypress oil in Epsom salt bath
42. Ginger chicken soup http://www.nourishingmeals.com/2011/02/healing-chicken-ginger-soup.html
Ayurvedic cleansing program (panchakarma)
Ginger tea with castor oil-by mouth
Simhanada guggulu-by mouth
Chitrak, and adhivati supplement-by mouth
Kaishore guggulu-by mouth
Cool castor oil
Cool coconut oil
Coconut Oil promotes optimal energy levels and supplies beneficial medium-chain triglycerides. It also promotes smoothe, supple skin in addition to:**
· Helping maintain the immune system.**
· Optimizing healthy metabolism.**
· Supporting weight management.**
Sandalwood Paste:
One of the most prized essential oils in aromatherapy, sandalwood oil is steam distilled from the fragrant wood of the East Indian sandalwood tree. In aromatherapy, this oil:
· Gently instills a sense of tranquility.
· Is a popular soothing meditative aid.
· Helps with quiet contemplation.
Ayurvedic dietary changes
Yoga
Breathing exercises
Amalaki tea
Other Tips for Ankylosing Spondylitis Pain Relief
Considering chiropractics?
Chiropractic treatment generally is NOT recommended for ankylosing spondylitis. “Chiropractic care isn’t advised for this type of back pain because changes from ankylosing spondylitis may increase the risk of injury during manipulation,” Ostrowski says. But there are a few other small steps you can take to help manage ankylosing spondylitis pain naturally. “I also recommend lots of deep breathing to keep your rib cage flexible, and I strongly advise against smoking," Ostrowski says. "Avoid physical and emotional stress as much as possible, have a good support system, and make sure to get enough rest.
"Sometimes with ankylosing spondylitis," she says, "you just need to take life a little slower.”