Prostate Cancer 101
How to Reduce Your Risk of Prostate Cancer
(or Even Reverse it)
Through Diet & Nutrition – Part 1
By Suresh Nair
This article first appeared in the July 2016 edition of TTAC’s Heroes Against Cancer member newsletter.
Prostate cancer is the second most common cancer affecting men, with nearly a million new cases diagnosed globally every year. It is also the second leading cause of death from cancer in men. Fortunately, prostate cancer has a nearly 90% survival rate after diagnosis.
Age, race, diet, lifestyle, environmental, and genetic factors are all believed to play a role in determining prostate cancer risk. According to the American Cancer Society, roughly one in seven American men will be diagnosed with prostate cancer during his lifetime. This cancer is typically seen in 60% or more of American men who are 65 years or older, but most men diagnosed with prostate cancer will not die from it.
Around 60% of men over the age of 65 will develop prostate cancer
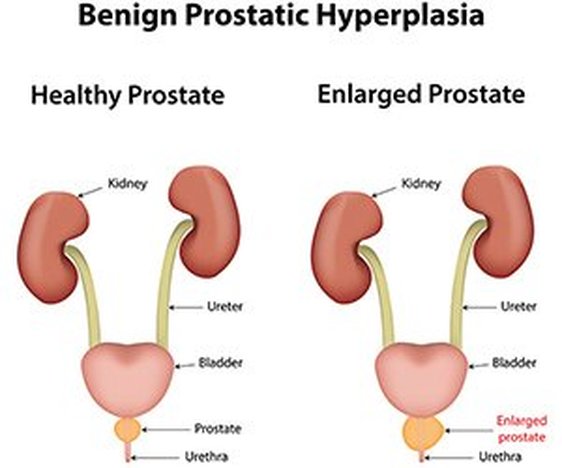
What is Benign Prostatic Hyperplasia (BPH)?
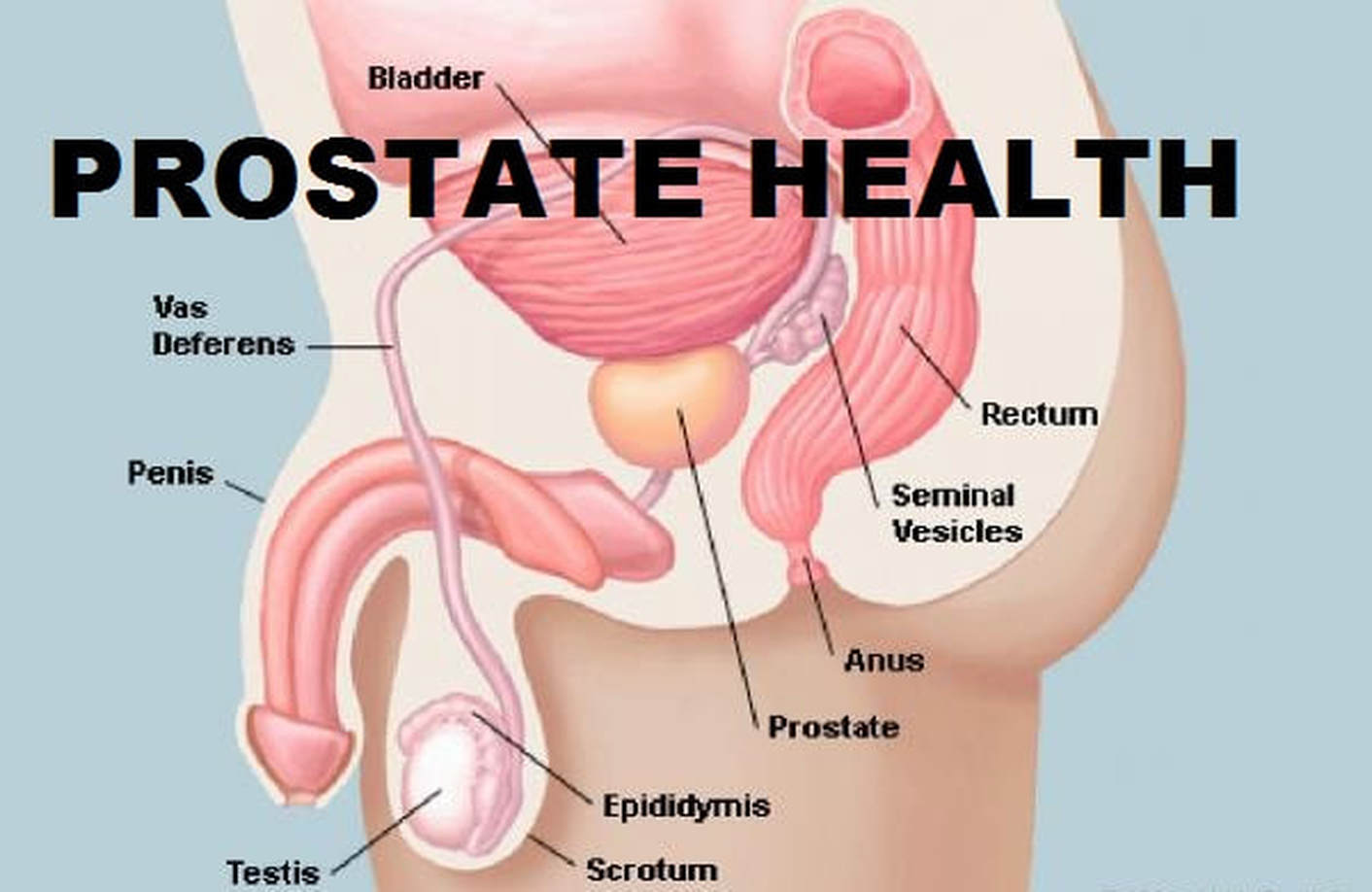
The prostate is about the size of a walnut and is located directly under the bladder in front of the rectum. It surrounds the urethra, the tube that carries urine and semen out of the body. Because of this, the prostate gland can affect urine control, known as continence.
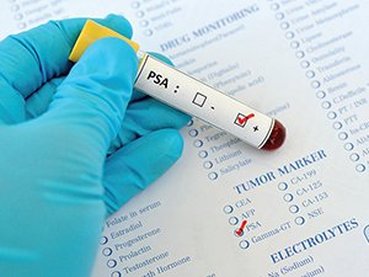
Thousands of tiny glands in the prostate make a fluid that forms semen, and also protects and nourishes the sperm. The prostate gland also makes a protein known as PSA (prostate-specific antigen), which helps to keep semen in a liquid state.
The prostate is about the size of a walnut and is located directly under the bladder in front of the rectum. It surrounds the urethra, the tube that carries urine and semen out of the body. Because of this, the prostate gland can affect urine control, known as continence.
Thousands of tiny glands in the prostate make a fluid that forms semen, and also protects and nourishes the sperm. The prostate gland also makes a protein known as PSA (prostate-specific antigen), which helps to keep semen in a liquid state.
An enlarged prostate often leads to
difficulty with urination
difficulty with urination
In some men the prostate grows bigger as they grow older, squeezing the urethra. Eventually the urethra may collapse, making it more difficult to pass urine. This condition is known as Benign Prostatic Hyperplasia (BPH).
BPH is considered to be a normal part of aging in men and is likely caused by changes in hormone levels. It can lead to:
In rare instances, BPH may block the bladder, making urination difficult or impossible. This can lead to bladder infections or stones, or even kidney damage.
However, it is important to remember that BPH does not cause prostate cancer. It also doesn’t affect a man’s ability to have children, nor does it cause erection problems.
Typical Prostate Cancer Symptoms
BPH is considered to be a normal part of aging in men and is likely caused by changes in hormone levels. It can lead to:
- Difficulties with getting urine started and completely stopped
- A frequent feeling of needing to urinate
- Weak urine stream
- The sense that the bladder has not completely emptied after urination
In rare instances, BPH may block the bladder, making urination difficult or impossible. This can lead to bladder infections or stones, or even kidney damage.
However, it is important to remember that BPH does not cause prostate cancer. It also doesn’t affect a man’s ability to have children, nor does it cause erection problems.
Typical Prostate Cancer Symptoms
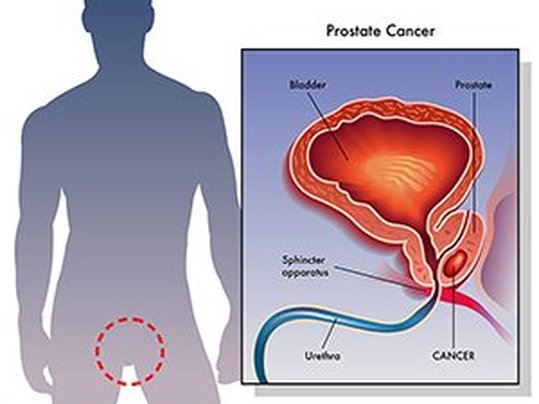
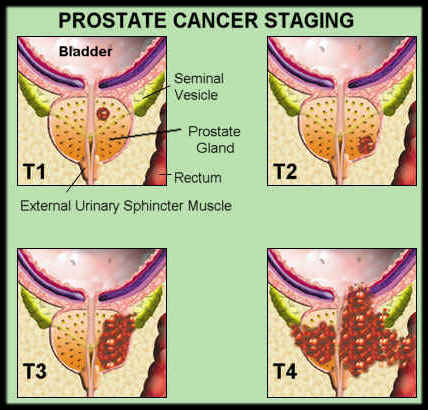
Prostate cancer develops when gland cells in the
prostate begin to grow uncontrollably.
prostate begin to grow uncontrollably.
Almost all prostate cancers are known as adenocarcinomas – this is the scientific name given to cancers that begin in cells that make and release mucus and other fluids.
Overall it is a very slow to moderately rapidly progressing disease. In fact, it is estimated that up to 80 percent of men in their eighties and older may have had prostate cancer when they died – without either them or their doctors knowing about it!
Often, people with prostate cancer do not experience any early symptoms.
Advanced prostate cancer can cause men to urinate more often or have a weaker flow of urine, but these symptoms can also be caused by non-cancerous prostate conditions. That being said, typical symptoms of prostate cancer include:
Fortunately, prostate cancer is one of the few cancers that can be completely cured, especially when it is localized to the prostate.
What is Metastatic Prostate Cancer?
Overall it is a very slow to moderately rapidly progressing disease. In fact, it is estimated that up to 80 percent of men in their eighties and older may have had prostate cancer when they died – without either them or their doctors knowing about it!
Often, people with prostate cancer do not experience any early symptoms.
Advanced prostate cancer can cause men to urinate more often or have a weaker flow of urine, but these symptoms can also be caused by non-cancerous prostate conditions. That being said, typical symptoms of prostate cancer include:
- Frequent urination
- Difficulty in starting or continuing urination
- Weak urine flow
- Blood in urine or semen
- Painful or burning urination
- Some combination of all these
Fortunately, prostate cancer is one of the few cancers that can be completely cured, especially when it is localized to the prostate.
What is Metastatic Prostate Cancer?
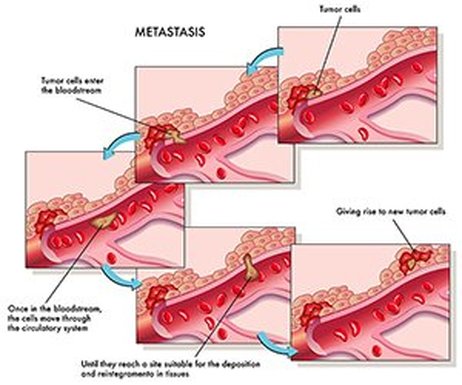
Prostate cancer is said to have become “metastatic” or “metastasized” when it spreads to other parts of the body from the prostate. Prostate cancer cells prefer to metastasize to lymph nodes, ribs, pelvic bones, and spine, although they may also spread to the liver or lungs. Very rarely they may also spread to other organs, such as the brain.
During metastasis, some cancer cells break away from the original tumor and move to a blood or lymph vessel, allowing them to move freely throughout the entire body. Eventually though they stop or get stuck in capillaries – which are tiny, narrow blood vessels – at some distant location.
Some of these cancer cells break through the capillary walls and attach themselves to nearby tissues or organs. If they succeed, they may start to grow – and eventually recruit new blood vessels to bring nutrients to feed themselves, creating a growing tumor.
Not all cancer cells that break away from their original site are able to form new tumors. Many don’t survive in the bloodstream. Others may die when they reach the new tissue, while still others just sit there for years, never becoming “active.”
It is estimated that roughly 50 percent of men diagnosed with local prostate cancer will develop metastatic cancer during their lifetime. However, this cancer responds to treatment even after metastasis – and some patients survive for many years even after the cancer has migrated to distant parts of the body. Clearly, the key is to catch prostate cancer early and manage it well. However, how exactly this needs to be done is the topic of a fierce, ongoing debate.
Prostate Cancer Detection: How Reliable is the PSA Test?
Most mainstream healthcare givers will advise that a man gets his prostate-specific antigen (PSA) levels tested regularly as the best way to catch prostate cancer early and remove or treat it safely.
However, are higher than normal PSA levels really suggestive of prostate cancer onset?
Should men with high PSA levels automatically allow themselves to get biopsied and undergo invasive treatments such as surgery and radiation therapy?
Not necessarily, because there is evidence to suggest that a biopsy or prostate removal can actually cause a dormant cancer to spread throughout the rest of the body. Not only that – according to recent evidence the PSA test may not be a reliable indicator of prostate cancer risk at all!
During metastasis, some cancer cells break away from the original tumor and move to a blood or lymph vessel, allowing them to move freely throughout the entire body. Eventually though they stop or get stuck in capillaries – which are tiny, narrow blood vessels – at some distant location.
Some of these cancer cells break through the capillary walls and attach themselves to nearby tissues or organs. If they succeed, they may start to grow – and eventually recruit new blood vessels to bring nutrients to feed themselves, creating a growing tumor.
Not all cancer cells that break away from their original site are able to form new tumors. Many don’t survive in the bloodstream. Others may die when they reach the new tissue, while still others just sit there for years, never becoming “active.”
It is estimated that roughly 50 percent of men diagnosed with local prostate cancer will develop metastatic cancer during their lifetime. However, this cancer responds to treatment even after metastasis – and some patients survive for many years even after the cancer has migrated to distant parts of the body. Clearly, the key is to catch prostate cancer early and manage it well. However, how exactly this needs to be done is the topic of a fierce, ongoing debate.
Prostate Cancer Detection: How Reliable is the PSA Test?
Most mainstream healthcare givers will advise that a man gets his prostate-specific antigen (PSA) levels tested regularly as the best way to catch prostate cancer early and remove or treat it safely.
However, are higher than normal PSA levels really suggestive of prostate cancer onset?
Should men with high PSA levels automatically allow themselves to get biopsied and undergo invasive treatments such as surgery and radiation therapy?
Not necessarily, because there is evidence to suggest that a biopsy or prostate removal can actually cause a dormant cancer to spread throughout the rest of the body. Not only that – according to recent evidence the PSA test may not be a reliable indicator of prostate cancer risk at all!
The PSA test is not a reliable indicator of prostate cancer as there
are many factors that can elevate PSA levels
are many factors that can elevate PSA levels
Instead, high PSA levels may only indicate that there’s inflammation in the body – which can include cancer, but not necessarily. It seems that general infections, benign swelling of the prostate including BPH, and even over-the-counter drugs can all elevate PSA levels.
In the U.S., most healthcare givers appear to be behind the curve, because in spite of the PSA test’s unreliability, prostate cancers are still diagnosed by screening with a PSA blood test or with a digital rectal examination. There is no clear evidence that either of these screening methods reduces the risk of death from prostate cancer – or that the benefits are greater than the harms of screening.
It is certainly true that these tests are able to detect prostate cancer at an early stage, but it doesn’t necessarily follow that earlier detection and subsequent treatment means better outcomes.
For instance, over 38,000 men were offered PSA testing for six 6 years and digital rectal examination for four years in the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. Another 38,000 men received usual care as the control group. After seven years, there was no difference in prostate cancer incidence between the screening and the control groups. Not only that, the rate of death from prostate cancer was very low and did not differ significantly between the two groups either.
While there is a clear trend toward lower mortality for prostate cancer in some countries, it’s unclear whether this trend is related to screening methods. Instead, other factors such as better and safer treatment modalities may be responsible.
How to Turn On “Tumor Killer Genes”
While the debate about the efficacy of prostate cancer screening rages on, a growing school of thought believes that a healthy diet, proper nutrition, and an active, healthy lifestyle may help to lower prostate cancer risk significantly. For instance, a pilot study on American men with low risk of prostate cancer found that following an intensive healthy diet and lifestyle regime – specifically, low meat and high vegetable and fruit intake, regular exercise, yoga, and meditation – can actually change how cancer progresses by turning on “tumor killer genes” and turning down or turning off the expression of so-called “tumor promoters.”
While most people understand the concept of eating healthy food, not everyone understands the role that proper nutrition plays in lowering disease risk. For instance, some studies suggest a predictive link between vitamin deficiency and cancer.
A vitamin is an organic compound (containing one or more carbon atoms) and is usually a vital nutrient that we require in limited amounts for our bodies to work properly. An organic compound or related set of compounds is called a vitamin when we cannot make it in our bodies in sufficient quantities, so that we are forced to get it in our diet. For example, ascorbic acid or vitamin C is a vitamin for humans because we cannot make it in our bodies at all. However, other animals can make enough and don’t need to get it in their diet, so it’s not a vitamin for them.
Let’s take a look at the role played by vitamins in prostate cancer risk, as shown by various scientific and clinical studies.
Why Getting Adequate Vitamin D is Vital
In the U.S., most healthcare givers appear to be behind the curve, because in spite of the PSA test’s unreliability, prostate cancers are still diagnosed by screening with a PSA blood test or with a digital rectal examination. There is no clear evidence that either of these screening methods reduces the risk of death from prostate cancer – or that the benefits are greater than the harms of screening.
It is certainly true that these tests are able to detect prostate cancer at an early stage, but it doesn’t necessarily follow that earlier detection and subsequent treatment means better outcomes.
For instance, over 38,000 men were offered PSA testing for six 6 years and digital rectal examination for four years in the Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial. Another 38,000 men received usual care as the control group. After seven years, there was no difference in prostate cancer incidence between the screening and the control groups. Not only that, the rate of death from prostate cancer was very low and did not differ significantly between the two groups either.
While there is a clear trend toward lower mortality for prostate cancer in some countries, it’s unclear whether this trend is related to screening methods. Instead, other factors such as better and safer treatment modalities may be responsible.
How to Turn On “Tumor Killer Genes”
While the debate about the efficacy of prostate cancer screening rages on, a growing school of thought believes that a healthy diet, proper nutrition, and an active, healthy lifestyle may help to lower prostate cancer risk significantly. For instance, a pilot study on American men with low risk of prostate cancer found that following an intensive healthy diet and lifestyle regime – specifically, low meat and high vegetable and fruit intake, regular exercise, yoga, and meditation – can actually change how cancer progresses by turning on “tumor killer genes” and turning down or turning off the expression of so-called “tumor promoters.”
While most people understand the concept of eating healthy food, not everyone understands the role that proper nutrition plays in lowering disease risk. For instance, some studies suggest a predictive link between vitamin deficiency and cancer.
A vitamin is an organic compound (containing one or more carbon atoms) and is usually a vital nutrient that we require in limited amounts for our bodies to work properly. An organic compound or related set of compounds is called a vitamin when we cannot make it in our bodies in sufficient quantities, so that we are forced to get it in our diet. For example, ascorbic acid or vitamin C is a vitamin for humans because we cannot make it in our bodies at all. However, other animals can make enough and don’t need to get it in their diet, so it’s not a vitamin for them.
Let’s take a look at the role played by vitamins in prostate cancer risk, as shown by various scientific and clinical studies.
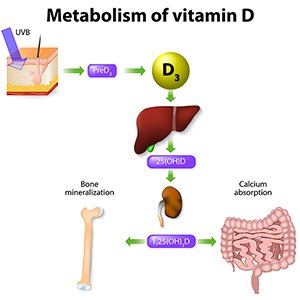
Why Getting Adequate Vitamin D is Vital
Known as the “sunshine vitamin,” up to 80-90 percent of the vitamin D we need is made in our body when our skin is exposed to sunlight – specifically to UVB radiation. The most important versions of vitamin D are vitamin D3 (cholecalciferol) and vitamin D2 (ergocalciferol). Very few foods contain vitamin D, because it only occurs naturally in low levels in some fatty fish, fish liver oils, and egg yolks. It is also present in fortified dairy and grain products.
Vitamin D is essential for strong bones because it helps the body absorb and use calcium from food. It is responsible for increasing intestinal absorption of calcium, iron, magnesium, phosphate, and zinc – and it also helps to maintain adequate blood levels of calcium and phosphate.
Traditionally, vitamin D deficiency has been associated with rickets, a disease in which the bone doesn’t properly mineralize, resulting in soft bones and skeletal deformities.
We know that vitamin D helps to improve muscle strength and immune function, along with reducing inflammation. However, it is only recently that the full extent of the role played by vitamin D in protecting us against disease has been revealed.
Specifically, vitamin D deficiency has been linked to a higher risk of developing up to 14 types of cancer, diabetes, heart disease, osteoporosis, rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, and autism – and quite possibly many more ailments that we don’t yet know of.
Multiple studies show that vitamin D deficiency increases prostate cancer risk. Vitamin D is transported in the blood by a protein known as vitamin D–binding protein (VDBP). In laboratory experiments, another protein made from VDBP known as VDBP-macrophage activating factor (VDBP-maf) has been shown to block the ability of prostate cancer cells to grow, migrate, and move from its original area to other parts of the body (metastasis).
In another interesting experiment, researchers examined tumor growth in a mouse model of prostate cancer in which the ability to use vitamin D had been blocked – and found that tumor growth in these mice was noticeably quicker than normal. Moving on to human studies, vitamin D levels were consistently found to be deficient over a period of 5 years in patients with non-metastatic prostate cancer.
In another study, patients with the lowest levels of 25-hydroxyvitamin D were seen to have a higher overall risk of developing metastatic prostate cancer. This result indicates that 25-hydroxyvitamin D may play a role in prostate cancer progression – and that it may even be a reliable prognostic marker in prostate cancer patients. (Note: 25-hydroxyvitamin D is a pre-hormone made in the liver from vitamin D3 (cholecalciferol). Measuring 25-hydroxyvitamin D levels is used to determine a person’s vitamin D status.)
In a case-control study, men who had lower vitamin D levels before prostate biopsy were more likely to have prostate cancer than men whose pre-biopsy vitamin D levels were higher.
Another study examined the potential link between vitamin D levels and survival in veterans. It found that veterans who were initially vitamin D deficient were significantly less likely to survive. Both initial and follow-up vitamin D deficiency meant a reduced likelihood of survival after prostate cancer diagnosis.
Another study with 1,447 cases of prostate cancer showed that men deficient in vitamin D had a 2-fold increased risk of advanced versus localized cancer and high-grade versus low-grade cancer. In other words, lower vitamin D levels were associated with having far more aggressive cancers.
Sunlight is by far the most reliable way of obtaining vitamin D. It comes as no surprise that men with low levels of sun exposure had an increased risk of prostate cancer. Interestingly however, among men who already had prostate cancer, less sun exposure was associated with lower risk of advanced disease.
Vitamin D is essential for strong bones because it helps the body absorb and use calcium from food. It is responsible for increasing intestinal absorption of calcium, iron, magnesium, phosphate, and zinc – and it also helps to maintain adequate blood levels of calcium and phosphate.
Traditionally, vitamin D deficiency has been associated with rickets, a disease in which the bone doesn’t properly mineralize, resulting in soft bones and skeletal deformities.
We know that vitamin D helps to improve muscle strength and immune function, along with reducing inflammation. However, it is only recently that the full extent of the role played by vitamin D in protecting us against disease has been revealed.
Specifically, vitamin D deficiency has been linked to a higher risk of developing up to 14 types of cancer, diabetes, heart disease, osteoporosis, rheumatoid arthritis, inflammatory bowel disease, multiple sclerosis, and autism – and quite possibly many more ailments that we don’t yet know of.
Multiple studies show that vitamin D deficiency increases prostate cancer risk. Vitamin D is transported in the blood by a protein known as vitamin D–binding protein (VDBP). In laboratory experiments, another protein made from VDBP known as VDBP-macrophage activating factor (VDBP-maf) has been shown to block the ability of prostate cancer cells to grow, migrate, and move from its original area to other parts of the body (metastasis).
In another interesting experiment, researchers examined tumor growth in a mouse model of prostate cancer in which the ability to use vitamin D had been blocked – and found that tumor growth in these mice was noticeably quicker than normal. Moving on to human studies, vitamin D levels were consistently found to be deficient over a period of 5 years in patients with non-metastatic prostate cancer.
In another study, patients with the lowest levels of 25-hydroxyvitamin D were seen to have a higher overall risk of developing metastatic prostate cancer. This result indicates that 25-hydroxyvitamin D may play a role in prostate cancer progression – and that it may even be a reliable prognostic marker in prostate cancer patients. (Note: 25-hydroxyvitamin D is a pre-hormone made in the liver from vitamin D3 (cholecalciferol). Measuring 25-hydroxyvitamin D levels is used to determine a person’s vitamin D status.)
In a case-control study, men who had lower vitamin D levels before prostate biopsy were more likely to have prostate cancer than men whose pre-biopsy vitamin D levels were higher.
Another study examined the potential link between vitamin D levels and survival in veterans. It found that veterans who were initially vitamin D deficient were significantly less likely to survive. Both initial and follow-up vitamin D deficiency meant a reduced likelihood of survival after prostate cancer diagnosis.
Another study with 1,447 cases of prostate cancer showed that men deficient in vitamin D had a 2-fold increased risk of advanced versus localized cancer and high-grade versus low-grade cancer. In other words, lower vitamin D levels were associated with having far more aggressive cancers.
Sunlight is by far the most reliable way of obtaining vitamin D. It comes as no surprise that men with low levels of sun exposure had an increased risk of prostate cancer. Interestingly however, among men who already had prostate cancer, less sun exposure was associated with lower risk of advanced disease.
Most people are not spending enough time in the sun
to produce adequate Vitamin D
to produce adequate Vitamin D
The geographic distribution of deaths because of prostate cancer is inversely related to UV radiation exposure. In other words, the more sunlight and UV radiation you’re exposed to, the lower your risk of developing and dying from this disease.
The sad reality is that vitamin D deficiency has reached epidemic proportions in the U.S. and many other parts of the world, simply because people do not spend enough time in the sun.
Get Your Vitamin D Levels Checked
To manage your risk for developing up to 14 forms of cancer and many other life-altering diseases, you need to regularly monitor and maintain 25-hydroxyvitamin D levels in your blood. Optimal vitamin D levels are between 60-100 ng/ml with the ideal range between 80-100 ng/ml for individuals looking to prevent or slow cancer growth. Having less than 50 ng/ml is considered to be vitamin D deficiency.
If you can, letting your own body make vitamin D from sun exposure is by far the easiest and the best way to optimize your vitamin D levels. However, occasional sun exposure to your face and hands is not enough for this. Instead, you need to expose large portions of your skin to the sun for an average of 10-20 minutes at a time.
Ultraviolet light from the sun comes in two main wavelengths – UVA and UVB. UVB is the healthy wavelength that helps your skin make vitamin D. Unlike UVA, UVB levels are low in morning and evening and high at midday. So to use the sun to maximize your vitamin D production, you need to expose your skin during the middle of the day. During this period most people with fair skin will make enough vitamin D with just 10-20 minutes of sun exposure. The darker your skin, the longer exposure you will need to optimize your vitamin D production.
Depending on where you live, this amount of sun exposure may be next to impossible, particularly through the winter months. As a result, supplementation is recommended for most. As a general guideline, take 1,000 IUs per 25 pounds (11.3 kg) of body weight to slowly raise your vitamin D levels into range or take 2,000 IUs per 25 pounds of body weight to quickly raise your vitamin D levels.
Because vitamin D is a fat-soluble nutrient, it is important to take the supplement with a fat-based meal for optimal absorption.
Research on the Impact of Vitamin E for Prostate Cancer Prevention
The sad reality is that vitamin D deficiency has reached epidemic proportions in the U.S. and many other parts of the world, simply because people do not spend enough time in the sun.
Get Your Vitamin D Levels Checked
To manage your risk for developing up to 14 forms of cancer and many other life-altering diseases, you need to regularly monitor and maintain 25-hydroxyvitamin D levels in your blood. Optimal vitamin D levels are between 60-100 ng/ml with the ideal range between 80-100 ng/ml for individuals looking to prevent or slow cancer growth. Having less than 50 ng/ml is considered to be vitamin D deficiency.
If you can, letting your own body make vitamin D from sun exposure is by far the easiest and the best way to optimize your vitamin D levels. However, occasional sun exposure to your face and hands is not enough for this. Instead, you need to expose large portions of your skin to the sun for an average of 10-20 minutes at a time.
Ultraviolet light from the sun comes in two main wavelengths – UVA and UVB. UVB is the healthy wavelength that helps your skin make vitamin D. Unlike UVA, UVB levels are low in morning and evening and high at midday. So to use the sun to maximize your vitamin D production, you need to expose your skin during the middle of the day. During this period most people with fair skin will make enough vitamin D with just 10-20 minutes of sun exposure. The darker your skin, the longer exposure you will need to optimize your vitamin D production.
Depending on where you live, this amount of sun exposure may be next to impossible, particularly through the winter months. As a result, supplementation is recommended for most. As a general guideline, take 1,000 IUs per 25 pounds (11.3 kg) of body weight to slowly raise your vitamin D levels into range or take 2,000 IUs per 25 pounds of body weight to quickly raise your vitamin D levels.
Because vitamin D is a fat-soluble nutrient, it is important to take the supplement with a fat-based meal for optimal absorption.
Research on the Impact of Vitamin E for Prostate Cancer Prevention
Good sources of vitamin E include olive oil, nuts,
seeds and egg yolks.
seeds and egg yolks.
Vitamin E was discovered in 1922 and occurs in 8 different forms – of these, alpha-tocopherol (the form commonly found in dietary supplements) is the most abundant in the body and the most biologically active. On the other hand, most dietary vitamin E is gamma-tocopherol.
Food sources of vitamin E include wheat germ, nuts, nut butters, seeds, egg yolks, olives and olive oil. Vegetable oils and margarine are also sources of vitamin E, however we recommend you avoid these products due to their inflammatory properties.
Studies suggest that vitamin E may protect against a number of chronic diseases, thanks to its actions as a powerful antioxidant. An antioxidant prevents or reduces the damage caused by reactive oxygen species (ROS) or free radicals. Free radicals react chemically with cellular structures such as DNA and proteins, damaging them and contributing to aging and chronic diseases such as diabetes, heart disease, and cancer.
The NIH-AARP Diet and Health Study set out to determine whether supplemental vitamin E and dietary gamma-tocopherol can prevent prostate cancer. Study participants filled out questionnaires and were followed for five years. At the end of the study, no association was found between vitamin E supplementation and prostate cancer risk. However, high consumption of dietary gamma-tocopherol was seen to lower the risk of advanced prostate cancer.
In another study, prostate cancer patients were seen to have significantly lower levels of vitamin E in their blood than healthy control subjects, although there is no evidence for cause and effect.
Participants in the Prostate, Lung, Colorectal and Ovarian (PLCO) Screening Trial were tested for blood levels of alpha-tocopherol and gamma-tocopherol, relative to their prostate cancer risk. An inverse relationship was observed between alphatocopherol levels and prostate cancer, but only in current and recently former smokers. In other words, the more alpha-tocopherol these people had in their blood, the lower their prostate cancer risk.
In the Physicians’ Health Study II, participants who were randomly assigned to receive 400 IU of synthetic alpha-tocopherol every other day for an average of 8 years had the same rates of prostate cancer as the control group, suggesting that vitamin E may not prevent prostate cancer.
Furthermore, vitamin E supplementation did not have an effect on deaths because of prostate cancer in these participants.
Other studies have suggested that genetic variations in specific genes may have an influence on the effect of alpha-tocopherol supplementation on prostate cancer risk. Clinical trials are ongoing to determine the efficacy and safety of various forms of vitamin E – both on its own and with other therapies – for prostate cancer treatment.
As you can see, there is no clear cut evidence yet for the exact role of vitamin E in determining prostate cancer risk. However, supplementation may lower your risk and provide some protection against more aggressive forms of prostate cancer. In any case, you want to ensure that you are not deficient in vitamin E.
Should Men Consider Modified Citrus Pectin (MCP) Supplementation to Lower Prostate Cancer Risk?
Strictly speaking, modified citrus pectin (MCP) is not part of everyone’s diet. Instead, citrus pectin is a complex carbohydrate found in the peel and pulp of citrus fruit that has traditionally been used as a thickening agent for jams and jellies. When “modified” by treatment with high pH and temperature, it dissolves better in water and is more readily absorbed by the body.
Preliminary research suggests that MCP may protect against various types of cancer, including colon, lung, and prostate cancer by inducing so-called “programmed cell death” or apoptosis, and by interfering with tumor cell metastasis (migration of tumor cells to other areas of the body).
MCP has also been shown to activate so-called “natural killer cells,” indicating that it may be able to boost immune system activity against cancer cells.
MCP is known to target galectin-3, a protein that is involved in the growth and migration of cancer cells to other parts of the body. MCP sticks to galectin-3, making the cell “slippery” and blocking the ability of galectin-3 to promote tumor growth and metastasis.
In a 2007 laboratory study, prostate cancer cells were treated with different pectins, including citrus pectin and fractionated pectin powder (FPP). While both killed the cancer cells, FPP induced more apoptosis than regular citrus pectin – suggesting that specific structural features of pectin may be responsible for its ability to induce apoptosis (cancer cell death) in prostate cancer cells.
Another study looked at the effects of MCP on the metastasis of prostate cancer cells injected into rats. Treatment with low to moderate doses reduced lung metastases but did not affect the growth of the main tumor.
In a 2007 study, patients with advanced solid tumors including prostate cancer received 5 grams of powdered MCP 3-times daily for eight weeks. Most patients in this study reported improvements in their physical functioning and overall health status, along with a reduction in fatigue, pain, and insomnia. Best of all, up to a quarter of these patients had stable disease after treatment.
If you think MCP will benefit you and you want to add it to your daily diet, experts recommend taking 1 teaspoon (5 g) three times daily of PectaSol-C, the only high quality brand of MCP that has been validated for purity.
Food sources of vitamin E include wheat germ, nuts, nut butters, seeds, egg yolks, olives and olive oil. Vegetable oils and margarine are also sources of vitamin E, however we recommend you avoid these products due to their inflammatory properties.
Studies suggest that vitamin E may protect against a number of chronic diseases, thanks to its actions as a powerful antioxidant. An antioxidant prevents or reduces the damage caused by reactive oxygen species (ROS) or free radicals. Free radicals react chemically with cellular structures such as DNA and proteins, damaging them and contributing to aging and chronic diseases such as diabetes, heart disease, and cancer.
The NIH-AARP Diet and Health Study set out to determine whether supplemental vitamin E and dietary gamma-tocopherol can prevent prostate cancer. Study participants filled out questionnaires and were followed for five years. At the end of the study, no association was found between vitamin E supplementation and prostate cancer risk. However, high consumption of dietary gamma-tocopherol was seen to lower the risk of advanced prostate cancer.
In another study, prostate cancer patients were seen to have significantly lower levels of vitamin E in their blood than healthy control subjects, although there is no evidence for cause and effect.
Participants in the Prostate, Lung, Colorectal and Ovarian (PLCO) Screening Trial were tested for blood levels of alpha-tocopherol and gamma-tocopherol, relative to their prostate cancer risk. An inverse relationship was observed between alphatocopherol levels and prostate cancer, but only in current and recently former smokers. In other words, the more alpha-tocopherol these people had in their blood, the lower their prostate cancer risk.
In the Physicians’ Health Study II, participants who were randomly assigned to receive 400 IU of synthetic alpha-tocopherol every other day for an average of 8 years had the same rates of prostate cancer as the control group, suggesting that vitamin E may not prevent prostate cancer.
Furthermore, vitamin E supplementation did not have an effect on deaths because of prostate cancer in these participants.
Other studies have suggested that genetic variations in specific genes may have an influence on the effect of alpha-tocopherol supplementation on prostate cancer risk. Clinical trials are ongoing to determine the efficacy and safety of various forms of vitamin E – both on its own and with other therapies – for prostate cancer treatment.
As you can see, there is no clear cut evidence yet for the exact role of vitamin E in determining prostate cancer risk. However, supplementation may lower your risk and provide some protection against more aggressive forms of prostate cancer. In any case, you want to ensure that you are not deficient in vitamin E.
Should Men Consider Modified Citrus Pectin (MCP) Supplementation to Lower Prostate Cancer Risk?
Strictly speaking, modified citrus pectin (MCP) is not part of everyone’s diet. Instead, citrus pectin is a complex carbohydrate found in the peel and pulp of citrus fruit that has traditionally been used as a thickening agent for jams and jellies. When “modified” by treatment with high pH and temperature, it dissolves better in water and is more readily absorbed by the body.
Preliminary research suggests that MCP may protect against various types of cancer, including colon, lung, and prostate cancer by inducing so-called “programmed cell death” or apoptosis, and by interfering with tumor cell metastasis (migration of tumor cells to other areas of the body).
MCP has also been shown to activate so-called “natural killer cells,” indicating that it may be able to boost immune system activity against cancer cells.
MCP is known to target galectin-3, a protein that is involved in the growth and migration of cancer cells to other parts of the body. MCP sticks to galectin-3, making the cell “slippery” and blocking the ability of galectin-3 to promote tumor growth and metastasis.
In a 2007 laboratory study, prostate cancer cells were treated with different pectins, including citrus pectin and fractionated pectin powder (FPP). While both killed the cancer cells, FPP induced more apoptosis than regular citrus pectin – suggesting that specific structural features of pectin may be responsible for its ability to induce apoptosis (cancer cell death) in prostate cancer cells.
Another study looked at the effects of MCP on the metastasis of prostate cancer cells injected into rats. Treatment with low to moderate doses reduced lung metastases but did not affect the growth of the main tumor.
In a 2007 study, patients with advanced solid tumors including prostate cancer received 5 grams of powdered MCP 3-times daily for eight weeks. Most patients in this study reported improvements in their physical functioning and overall health status, along with a reduction in fatigue, pain, and insomnia. Best of all, up to a quarter of these patients had stable disease after treatment.
If you think MCP will benefit you and you want to add it to your daily diet, experts recommend taking 1 teaspoon (5 g) three times daily of PectaSol-C, the only high quality brand of MCP that has been validated for purity.
“Pectin” is a carbohydrate substance that is found naturally in the inner cell wall of most plants. It is especially concentrated in the peel and pulp of citrus fruits, including grapefruits, oranges, limes, and lemons
Conclusions
So far we’ve looked at two vital nutrients, Vitamin D and Vitamin E, and what research has found their role to be in regard to prostate cancer risk. In general, studies show that DEFICIENCY of either of these vitamins is associated with a greater risk of developing prostate cancer, or more aggressive forms of prostate cancer. However, the precise connection between levels of these two vitamins in the blood and prostate cancer risk have not yet been completely understood.
Preliminary research also suggests that modified citrus pectin (MCP) may protect against colon, lung, and prostate cancer by inducing so-called “programmed cell death” or apoptosis, and by interfering with metastasis, or migration of cancer cells from the original area to other parts of the body.
In Part 2 of this series we’ll examine how diet impacts prostate cancer risk and progression of the disease, as well as recommended foods to incorporate as part of a prevention or treatment program.
This article first appeared in the July 2016 edition of TTAC’s Heroes Against Cancer newsletter. Each month in Heroes Against Cancer we share the best ways you can use to get and stay healthy – including delicious recipes and the best in supplements, herbs, and spices. Find out more about our member newsletter here.
Article Summary
So far we’ve looked at two vital nutrients, Vitamin D and Vitamin E, and what research has found their role to be in regard to prostate cancer risk. In general, studies show that DEFICIENCY of either of these vitamins is associated with a greater risk of developing prostate cancer, or more aggressive forms of prostate cancer. However, the precise connection between levels of these two vitamins in the blood and prostate cancer risk have not yet been completely understood.
Preliminary research also suggests that modified citrus pectin (MCP) may protect against colon, lung, and prostate cancer by inducing so-called “programmed cell death” or apoptosis, and by interfering with metastasis, or migration of cancer cells from the original area to other parts of the body.
In Part 2 of this series we’ll examine how diet impacts prostate cancer risk and progression of the disease, as well as recommended foods to incorporate as part of a prevention or treatment program.
This article first appeared in the July 2016 edition of TTAC’s Heroes Against Cancer newsletter. Each month in Heroes Against Cancer we share the best ways you can use to get and stay healthy – including delicious recipes and the best in supplements, herbs, and spices. Find out more about our member newsletter here.
Article Summary
- Prostate cancer is the second most common cancer affecting men. It is also the second leading cause of death from cancer in men. Prostate cancer has a nearly 90% survival rate after diagnosis, however.
- In some men the prostate grows bigger as they grow older, squeezing the urethra (the tube that carries urine & semen out of a man’s body). Eventually the urethra may collapse, making it more difficult to pass urine. This condition is known as Benign Prostatic Hyperplasia (BPH).
- BPH does NOT cause prostate cancer. Prostate cancer develops when gland cells in the prostate begin to grow uncontrollably.
- Typical symptoms of prostate cancer include:
- Frequent urination
- Difficulty in starting or continuing urination
- Weak urine flow
- Blood in urine or semen
- Painful or burning urination
- Some combination of all these
- Prostate cancer is said to have become “metastatic” or “metastasized” when it spreads to other parts of the body from the prostate. Prostate cancer cells prefer to metastasize to lymph nodes, ribs, pelvic bones, and spine, although they may also spread to the liver or lungs.
- Approximately 50% of men diagnosed with local prostate cancer will develop metastatic cancer during their lifetime. However, this cancer responds to treatment even after metastasis. The key is to catch prostate cancer early and manage it well.
- There is no clear evidence that either PSA testing or a digital rectal exam reduces the risk of death from prostate cancer – or that the benefits are greater than the harms of screening.
- A growing school of thought believes that a healthy diet, proper nutrition, and an active, healthy lifestyle may help to lower prostate cancer risk significantly
- Vitamin D deficiency has been linked to a higher risk of developing up to 14 types of cancer – including prostate cancer – as well as many other serious diseases.
- While there is no clear cut evidence for the role of vitamin E in determining prostate cancer risk, supplementation may lower risk and provide some protection against more aggressive forms of prostate cancer. In any case, ensure you’re are not deficient in vitamin E.
- Modified Citrus Pectin (MCP) has been shown to activate so-called “natural killer cells,” indicating that it may be able to boost immune system activity against cancer cells.
Sources and References
About the Author: Suresh Nair is a health writer with more than 15 years of experience as a practicing laboratory scientist. He is also a former copy-editor and project manager at a medical communications company. Suresh has written hundreds of articles on health, alternative health, fitness, and nutrition as well as various other medical and clinical topics. As a scientist (with a PhD in Molecular Neurobiology from UPenn), his articles are always thoroughly researched and have a sound scientific basis.
Read Part 2 Here
- Mortality results from a randomized prostate-cancer screening trial
- Clinical Benefit in Patients with Advanced Solid Tumors Treated with Modified Citrus Pectin: A Prospective Pilot Study
- 4 Early Warning Signs of Prostate Cancer
- Vitamin D and prostate cancer survival in veterans
- Vitamins E and C in the prevention of prostate and total cancer in men: the Physicians’ Health Study II randomized controlled trial
- Associations of circulating 25-hydroxyvitamin D with prostate cancer diagnosis, stage and grade
- Vitamin D binding protein-macrophage activating factor directly inhibits proliferation, migration, and uPAR expression of prostate cancer cells
- Effects of daily oral administration of quercetin chalcone and modified citrus pectin on implanted colon-25 tumor growth in Balb-c mice
- Pectin induces apoptosis in human prostate cancer cells: correlation of apoptotic function with pectin structure
- Tumor progression in the LPB-Tag transgenic model of prostate cancer is altered by vitamin D receptor and serum testosterone status
- Prostate Cancer: Causes, Symptoms and Treatments
- Nutrition, dietary interventions and prostate cancer: the latest evidence
- Inhibition of spontaneous metastasis in a rat prostate cancer model by oral administration of modified citrus pectin
- Activation of human T-helper/inducer cell, T-cytotoxic cell, B-cell, and natural killer (NK)-cells and induction of natural killer cell activity against K562 chronic myeloid leukemia cells with modified citrus pectin
- UV, latitude, and spatial trends in prostate cancer mortality: all sunlight is not the same (United States)
- Calpain activation through galectin-3 inhibition sensitizes prostate cancer cells to cisplatin treatment
- Serum α-tocopherol and γ-tocopherol concentrations and prostate cancer risk in the PLCO Screening Trial: a nested case-control study
- What Is Metastatic Prostate Cancer?”
- Supplemental and dietary vitamin E intakes and risk of prostate cancer in a large prospective study
About the Author: Suresh Nair is a health writer with more than 15 years of experience as a practicing laboratory scientist. He is also a former copy-editor and project manager at a medical communications company. Suresh has written hundreds of articles on health, alternative health, fitness, and nutrition as well as various other medical and clinical topics. As a scientist (with a PhD in Molecular Neurobiology from UPenn), his articles are always thoroughly researched and have a sound scientific basis.
Read Part 2 Here
********************
medical professionals
Learn How to USE HYPOCHLOROUS Acid (HOCL)
Safely & Effectively.
Get A HYPOCHLOROUS acid (HOCL)
Private Use Consultation.
special rate for medical professionals
(Telephone Consultations ONLY)
With medical missionary
In order to keep our content free, some of the links maybe affiliate links to trusted websites and products we enjoy using. Shopping through these links will in some cases give you a discount and also bring a small commission to JAHealthAdvocate.com. Read our full Affiliate Disclosure for more info.
Terms of Use: DMCA: Privacy Policy: Disclaimer: Sitemap: Comments Policy:
Affiliate Disclosure: Advertising: Our Beliefs: PMA
|
TOP NATURAL CANCER PROTOCOLS Follow Us:
|
Our VisitorsDo you like the info we share here? Was it of benefit to you? Support our efforts with a donation. Let's keep the information flowing. Any amount helps. Thank you.
|
| ||||||
Amare EDGE
AFFILIATE DISCLOSURE
LEGAL DISCLAIMER & SAFETY INFORMATION: The content of this JA Health Advocate Website is presented for educational purposes only, and is not intended to diagnose or prescribe for any medical or psychological condition, nor to prevent, treat, mitigate or cure such conditions.
This information (and any accompanying material) is not intended to replace the attention or advice of a physician or other qualified health care professional.
Anyone who wishes to embark on any dietary, drug, exercise, or other lifestyle change intended to prevent or treat a specific disease or condition should first consult with and seek clearance from a physician or other qualified health care professional. Pregnant women in particular should seek the advice of a physician before using any protocol listed on this website.
The protocols described on this website are for adult use only, unless otherwise specified. Protocol or product labels may contain important safety information and the most recent information provided by the linked product manufacturers, should be carefully reviewed prior to use to verify the usage rate, administration, and contraindications.
National, state, and local laws may vary regarding the use and application of many of the therapies discussed. The reader assumes the risk of any injuries. The authors and publishers, their affiliates and assigns are not liable for any injury and/or damage to persons arising from ANY protocols listed on this website, and expressly disclaim responsibility for any adverse effects resulting from the use of the information contained herein.
The protocols raise many issues that are subject to change as new data emerge. None of our suggested protocol regimens can guarantee health benefits. JA Health Advocate has not performed independent verification of the data contained in the referenced materials, and expressly disclaims responsibility for any error in any of the shared literature.
The information contained herein is not intended to replace a one-on-one relationship with a doctor or qualified healthcare professional. Therefore, this information is not intended as medical advice, but rather a sharing of knowledge and information based on research and experience. JA Health Advocate encourages you to make your own health care decisions based on your judgment and research in partnership with a qualified healthcare professional.
The CLO2 Protocols described on this site are for informational purposes ONLY. The reader accepts 100% responsibility for any and all use made of any information herein.
These statements have not been evaluated by the US Food and Drug Administration or the Jamaica Ministry of Health. The information on this website is not intended to diagnose, treat, cure or prevent any disease. They should not replace personal judgment nor medical treatment, nor are they intended to diagnose, treat, cure, or prevent any disease. Always talk to your Natural Health Provider or M.D. about the use of these or any other complimentary modalities. Reading this website denotes your understanding and agreement to our full disclaimer.
You should contact a trained professional who understands how to safely and effectively use CLO2 and it's derivatives.
This information (and any accompanying material) is not intended to replace the attention or advice of a physician or other qualified health care professional.
Anyone who wishes to embark on any dietary, drug, exercise, or other lifestyle change intended to prevent or treat a specific disease or condition should first consult with and seek clearance from a physician or other qualified health care professional. Pregnant women in particular should seek the advice of a physician before using any protocol listed on this website.
The protocols described on this website are for adult use only, unless otherwise specified. Protocol or product labels may contain important safety information and the most recent information provided by the linked product manufacturers, should be carefully reviewed prior to use to verify the usage rate, administration, and contraindications.
National, state, and local laws may vary regarding the use and application of many of the therapies discussed. The reader assumes the risk of any injuries. The authors and publishers, their affiliates and assigns are not liable for any injury and/or damage to persons arising from ANY protocols listed on this website, and expressly disclaim responsibility for any adverse effects resulting from the use of the information contained herein.
The protocols raise many issues that are subject to change as new data emerge. None of our suggested protocol regimens can guarantee health benefits. JA Health Advocate has not performed independent verification of the data contained in the referenced materials, and expressly disclaims responsibility for any error in any of the shared literature.
The information contained herein is not intended to replace a one-on-one relationship with a doctor or qualified healthcare professional. Therefore, this information is not intended as medical advice, but rather a sharing of knowledge and information based on research and experience. JA Health Advocate encourages you to make your own health care decisions based on your judgment and research in partnership with a qualified healthcare professional.
The CLO2 Protocols described on this site are for informational purposes ONLY. The reader accepts 100% responsibility for any and all use made of any information herein.
These statements have not been evaluated by the US Food and Drug Administration or the Jamaica Ministry of Health. The information on this website is not intended to diagnose, treat, cure or prevent any disease. They should not replace personal judgment nor medical treatment, nor are they intended to diagnose, treat, cure, or prevent any disease. Always talk to your Natural Health Provider or M.D. about the use of these or any other complimentary modalities. Reading this website denotes your understanding and agreement to our full disclaimer.
You should contact a trained professional who understands how to safely and effectively use CLO2 and it's derivatives.
Anyone considering the use of chlorine dioxide (CLO2) needs to be aware the US Food and Drug Administration has issued a Consumer Update warning against the use of chlorine dioxide, see https://www.fda.gov/consumers/consumer-updates/danger-dont-drink-miracle-mineral-solution-or-similar-products. This warning and this stance taken by a government agency should be considered carefully by everyone.
The chemicals must be handled with respect. In addition, usage rates and guidelines must be understood and followed carefully. Many individuals have found they can learn to use chlorine dioxide effectively, but this has yet to be recognized by government authorities. The recommendation is for you to find a doctor who will be on board and be supportive of using any of the self-help techniques you may find on this site.
The chemicals must be handled with respect. In addition, usage rates and guidelines must be understood and followed carefully. Many individuals have found they can learn to use chlorine dioxide effectively, but this has yet to be recognized by government authorities. The recommendation is for you to find a doctor who will be on board and be supportive of using any of the self-help techniques you may find on this site.
The FDA Considers MMS/CD - Chlorine Dioxide as SAFE for Humans
FDA Patents for MMS/CD - Chlorine Dioxide for Cancer Care
FDA Patent: Chlorine dioxide gas for use in treating respiratory virus infection
FDA Patent: Apparatus and method for disinfecting water
FDA Patent for HIV Treatment
FDA Patent for inflammatory diseases
FDA Patents for MMS/CD - Chlorine Dioxide for Cancer Care
FDA Patent: Chlorine dioxide gas for use in treating respiratory virus infection
FDA Patent: Apparatus and method for disinfecting water
FDA Patent for HIV Treatment
FDA Patent for inflammatory diseases
We do not sell products, but we do supply you with links
to approved suppliers who we buy from too.
Copyright © 2020 JA Health Advocate · All Rights Reserved · Powered by DebsWebDesign